Executive Summary
In the wake of the 2022 U.S. Supreme Court decision in Dobbs v. Jackson Women’s Health Organization, Oklahoma residents are currently living under three overlapping and inconsistent state abortion bans that, if violated, impose severe civil and criminal penalties on health care providers. Exceptions to these new laws, enacted around the Supreme Court’s overturning of its 1973 ruling in Roe v. Wade, are extremely limited and confusing to health professionals and potential patients alike. Because the exceptions drafted by legislators are often conflicting and use non-medical terminology, they sow confusion around what kinds of care and procedures health care providers can legally offer when a pregnancy threatens a person’s health or life. These challenges, combined with the significant penalties under these bans, constitute a situation of “dual loyalty”: health professionals are forced to balance their obligation to provide ethical, high-quality medical care against the threat of legal and professional sanctions. The decision to provide emergency medical care risks becoming a legal question – determined by lawyers – rather than a question of clinical judgment and the duty of care to the patient – determined by health care professionals.
In light of the extensive anti-abortion legal framework newly in place in the state, Oklahoma offers an important insight into the potential effects of near-total abortion bans on pregnant patients and the clinicians who care for them. While bans such as Oklahoma’s have already severely limited access to abortion medication or procedures, reproductive justice advocates have raised concerns that it is especially unclear what care remains accessible in practice in cases of obstetric emergencies. Accordingly, Physicians for Human Rights (PHR), Oklahoma Call for Reproductive Justice (OCRJ), and the Center for Reproductive Rights (CRR) have examined Oklahoma as a case study to investigate two key questions:
- Do hospitals have policies and/or protocols that govern decision-making when pregnant people face medical emergencies, and are pregnant people in Oklahoma able to receive information on these policies, if they do exist?
- If information is provided to prospective patients on hospital policies and/or protocols related to obstetric emergency care, what is the content and quality of that information?
To study these questions, PHR, OCRJ, and CRR used a “simulated patient” research methodology, in which research assistants posed as prospective patients and called hospitals that provide prenatal and peripartum care across the state of Oklahoma to ask questions related to emergency pregnancy care.
Not a single hospital in Oklahoma appeared to be able to articulate clear, consistent policies for emergency obstetric care that supported their clinicians’ ability to make decisions based solely on their clinical judgement and pregnant patients’ stated preferences and needs.
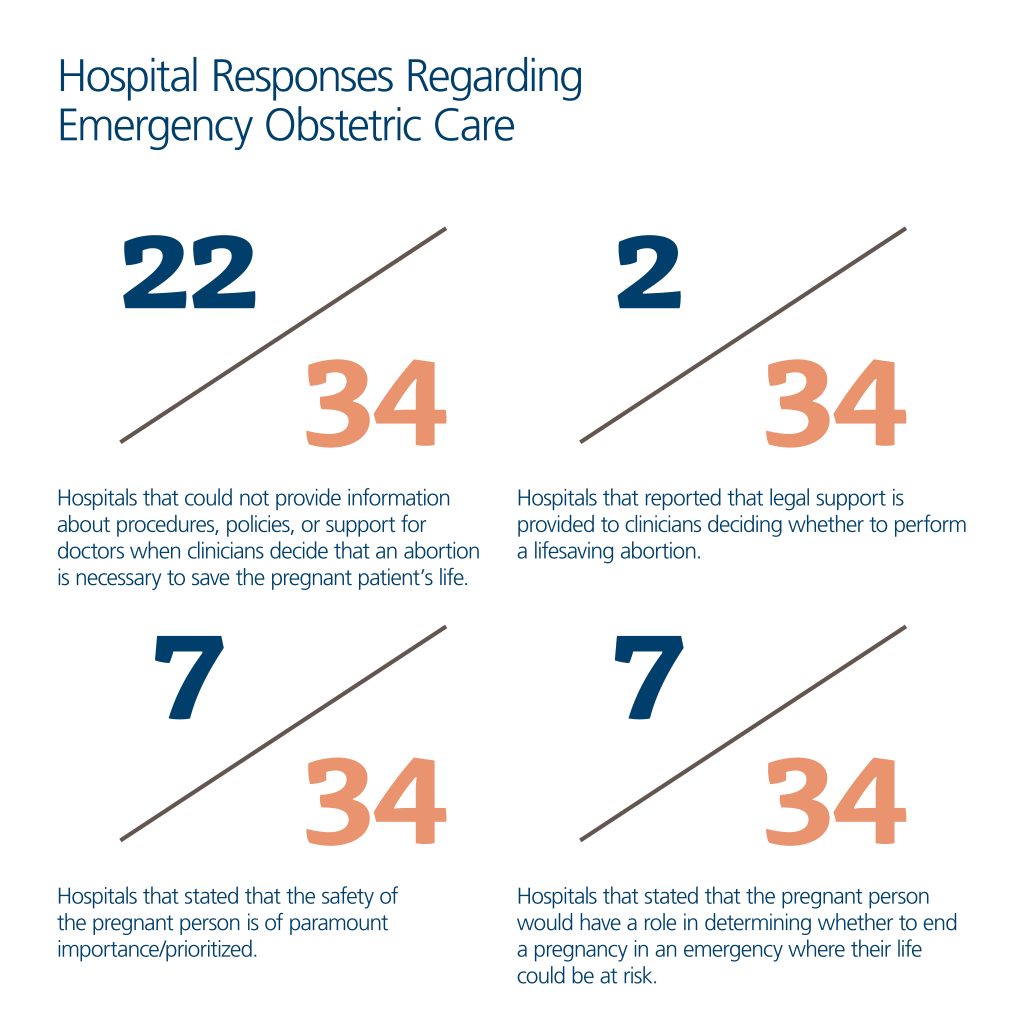
The results of this research are alarming. Not a single hospital in Oklahoma appeared to be able to articulate clear, consistent policies for emergency obstetric care that supported their clinicians’ ability to make decisions based solely on their clinical judgement and pregnant patients’ stated preferences and needs. Of the 34 out of 37 hospitals offering obstetric care across the state of Oklahoma that were reached, 65 percent (22 hospitals) were unable to provide information about procedures, policies, or support provided to doctors when the clinical decision is that it is necessary to terminate a pregnancy to save the life of a pregnant patient; only two hospitals described providing legal support for clinicians in such situations. In 14 cases (41 percent), hospital representatives provided unclear and/or incomplete answers about whether doctors require approval to perform a medically necessary abortion. Three hospitals indicated that they have policies for these situations but refused to share any information about them; four stated they have approval processes that clinicians must go through if they deem it necessary to terminate a pregnancy; and three stated that their hospitals do not provide abortions at all. (Oklahoma hospitals that are affiliated with an Indigenous nation were excluded from the study; because they operate under federal oversight, it is unclear how the Oklahoma bans impact them.) Some examples of the information the simulated patients received include:
- One hospital representative claimed: “If the situation is truly life-threatening, decisions will be made,” without explaining how those decisions would be made or by whom.
- Another hospital representative stated that, “[i]t is tricky because of state laws, but we will not let the mom die.”
- In one circumstance, the caller was told that a pregnant patient’s body would be used as an “incubator” to carry the baby as long as possible.
- At one hospital, a staff member put the simulated caller on hold and, after consulting with a hospital physician, told the caller, “Nowhere in the state of Oklahoma can you get an abortion for any reason,” even though the bans have exceptions.
In sum, in response to questioning, hospitals provided opaque, contradictory, and incorrect information about when an abortion is available; lacked clarity on criteria and approval processes for abortions; and offered little reassurance to patients that their survival would be prioritized or that their perspectives would be considered.
Hospitals provided opaque, contradictory, and incorrect information about when an abortion is available; lacked clarity on criteria and approval processes for abortions; and offered little reassurance to patients that their survival would be prioritized or that their perspectives would be considered.
The study’s findings demonstrate that despite apparently good-faith efforts from most hospital representatives, callers could not access clear and accurate information about the care they would receive if facing a pregnancy-related medical emergency at any given institution. Moreover, the information they received was often confusing – at some hospitals, callers received conflicting information from separate staff within the same hospital. These findings raise grave concerns about the ability of a pregnant person in Oklahoma – and the other 12 states with similar, near-total abortion bans – to receive clear, sufficient, and necessary information to make informed decisions about their medical care, as well as the ability of such patients to receive medically-necessary treatment. Callers also found that some hospital administrations, in an effort to comply with state laws, imposed restrictive policies on medical personnel that would impede their ability to provide prompt and effective care for pregnant patients with medical emergencies, including in cases of miscarriage.
One hospital representative claimed: “If the situation is truly life-threatening, decisions will be made,” without explaining how those decisions would be made or by whom. In one circumstance, the caller was told that a pregnant patient’s body would be used as an “incubator” to carry the baby as long as possible.
Health care providers face a similarly untenable situation under the current abortion bans. The criminalization of abortion denies access to abortion for pregnant people under most circumstances, and narrow exceptions such as “only to save the life” of the pregnant patient lead to confusion, uncertainty, and fear, both for pregnant people and for the hospitals and health care providers that care for them. Clinicians face severe criminal and civil penalties, such as the loss of their medical licenses and long prison sentences, if prosecutors and state legislators disagree with their medical decision-making. In light of these obstacles, pregnant people are faced with the frightening possibility that they will be unable to receive science-informed, patient-centered, and ethical medical care should they face an obstetric emergency.
These results reflect how Oklahoma’s abortion bans threaten the health and well-being of pregnant people and violate their human rights. These violations include individuals’ rights to life, health, equality, information, freedom from torture and ill-treatment, and to exercise reproductive autonomy. These findings further affirm what has been recognized by the World Health Organization: that the criminalization and penalization of abortion care – even with an exception for medical necessity – is fundamentally inconsistent with evidence-based, ethical, and patient-centered health care.
Oklahoma’s abortion bans threaten the health and well-being of pregnant people and violate their human rights.
Given these findings, PHR, OCRJ, and CRR make the following topline recommendations: (full recommendations can be found below)
To the Oklahoma Legislature:
- Repeal Oklahoma’s abortion bans and decriminalize abortion.
- Ensure that health care services for pregnant people and all Oklahomans are accessible and of good quality.
To Oklahoma’s Hospitals and Health Care Professionals:
- Speak out against laws criminalizing abortion or otherwise restricting access to abortions, including during obstetric emergencies.
- Build knowledge and awareness of professional recommendations and guidance for providing abortion services.
To State and National Medical Associations:
- Publicly condemn abortion bans and continue to speak out against the dual loyalty impacts of abortion bans, including citing evidence of how such laws undermine ethical obligations and professional duties of care.
To the Federal Government:
- Enact and implement national laws and policies that ensure rights and remove barriers to abortion care and maternal health care.

Introduction
In June 2022, the U.S. Supreme Court issued its decision in Dobbs v. Jackson Women’s Health Organization overturning almost 50 years of legal precedent and eliminating the federal constitutional right to abortion. This decision marked the first time in American history that the Supreme Court took away a right it had recognized as fundamental to personal liberty. As U.S. Attorney General Merrick Garland noted, abortion has been “an essential component of women’s liberty for half a century – a right that has safeguarded women’s ability to participate fully and equally in society.”[1]
Oklahoma was one of many states that sought to ban abortion in the lead-up to – and in the wake of – the Dobbs decision. It now has three overlapping abortion bans in effect, each with different elements and exceptions. A fourth ban with criminal penalties was enacted in 2022, but that law was struck down by the Oklahoma Supreme Court in March 2023. Providing someone with an abortion or assisting them in accessing an abortion in Oklahoma remains illegal, except in narrowly and ambiguously defined medical emergencies and circumstances that threaten a pregnant person’s life.[2] State legislators in Oklahoma continued to push legislation in 2023 that creates further legal risk for those involved in receiving and providing care for pregnant people in cases of emergencies.
In light of the many anti-abortion laws enacted in recent years in the state, Oklahoma offers an important view into the potential effects of near-total abortion bans on pregnant patients and the clinicians who care for them, both in Oklahoma and in other states with similar bans. Using a “simulated patient” research methodology, this study examined whether pregnant people could access information about the care they might receive at Oklahoman hospitals that provide prenatal and peripartum care, should they face a medical emergency – and, if they could, the quality and clarity of that information.

The Effect of Dobbs on Abortions Provided Due to a Medical Emergency
In the wake of the Dobbs decision, a number of states swiftly began instituting or enforcing laws that nearly or entirely ban abortion with narrow exceptions, many with criminal penalties for health professionals who provide abortion care. As of April 2023, 13 states have instituted and are enforcing abortion bans.[3] For example, Arkansas bans abortions at all stages of pregnancy, with no exemptions except to “save the life” of a pregnant person.[4] Mississippi similarly bans abortion with narrow exceptions to “save the life” of a pregnant person or in cases of rape or incest that are reported to law enforcement.[5] South Dakota bans abortions with exceptions to “preserve the life” of a pregnant person.[6] The impact of these laws will fall hardest on people who already face discriminatory obstacles to health care: Black, Indigenous, and other people of color, people with disabilities, people in rural areas, young people, undocumented people, and those with limited financial resources.[7]
Many of these states’ laws contain language that does not reflect precise or accurate medical terminology, particularly in describing valid legal exemptions to the bans. Of particular concern, as of February 21, 2023, four out of the 13 states with abortion bans include exemptions phrased along the lines of, “except when necessary to save the life of the mother,” with no further detail, explanation, or other exemptions.[8] Four other states use this language and add only one additional exception written along the lines of, “to prevent severe, permanent damage to major organs or bodily functions.”[9]
In practice, the language used for exceptions to abortion bans is open to interpretation. This may seem like a positive measure – giving deference to clinicians in applying laws. However, against a backdrop of criminalization and inconsistent exceptions that do not utilize medical language, such exceptions only sow more fear and confusion and potentially make clinicians reluctant to take steps to provide necessary medical care to patients.[10] For instance, what circumstances or indicators of medical severity qualify as an emergency that threatens a pregnant person’s life? How imminent or severe must the threat be? What are appropriate mechanisms and policies that health systems must enact to provide support, guidance, and legal protection for health professionals faced with these time-sensitive and critical clinical decisions? To what extent are or should a patient’s own views and tolerance for risk be considered in such decision-making?
These narrow, vague exceptions to criminalization place medical professionals providing care for pregnant patients in the position of balancing their duty to provide ethical, high-quality medical care against the threat of legal and professional sanctions. In other words, physicians must weigh concerns for their patients’ health with the recognition that their actions in medical emergencies could leave them vulnerable to criminal charges, with potential penalties as severe as 15 years in prison, thousands of dollars in fines, and loss of their medical licenses. Such conflicts constitute dual loyalty, a situation in which health care workers “find their obligations to their patients in direct conflict with their obligations to a third party … that holds authority over them” – in this case, state governments.[11]
Physicians must weigh concerns for their patients’ health with the recognition that their actions in medical emergencies could leave them vulnerable to criminal charges, with potential penalties as severe as 15 years in prison, thousands of dollars in fines, and loss of their medical licenses.
This concern has quickly proven true. American Medical Association President Jack Resneck, Jr. has decried the “chaos” into which health care has been thrust since the Dobbs decision, describing physicians as “caught between good medicine and bad law,” struggling to “meet their ethical duties to patients’ health and well-being, while attempting to comply with reckless government interference in the practice of medicine that is dangerous to the health of … patients…. Physicians and other health care professionals must attempt to comply with vague, restrictive, complex, and conflicting state laws that interfere in the practice of medicine.”[12]
American Medical Association President Jack Resneck, Jr. has decried the “chaos” into which health care has been thrust since the Dobbs decision, describing physicians as “caught between good medicine and bad law.”
Providers have shared concerns about confusion related to medical emergencies and the incompatibility of various state abortion laws with caring for patients facing such emergencies. Tennessee has an abortion ban with no exceptions, although it allows providers to raise a defense in a prosecution that an abortion was medically necessary. Seven hundred doctors signed on to a letter calling on legislators to reconsider the ban for a variety of reasons, including because “it forces health care providers to balance appropriate medical care with the risk of criminal prosecution.”[13] Similarly, Louisiana doctors who are operating under several bans attested that “[f]ear of punishment aligned with lack of clarity on how this law will be enforced can lead to devastating consequences for Louisiana women as well as moral distress for the clinicians who care for them and have taken the Hippocratic oath to do no harm.”[14] Common pregnancy complications may present situations where providers are too cautious in providing necessary care because they are concerned that a patient is not sick enough, such as if a patient presents with preterm premature rupture of membranes (i.e., when the amniotic sac surrounding the fetus prematurely ruptures), potentially serious infections, or with other preterm complications that require emergency medical intervention and are likely to result in pregnancy loss or long-term harm to the pregnant person’s health and reproductive capacity.[15]
The bans also have concerning implications for the medical management of miscarriages (threatened, incomplete, or complete). It is estimated that up to 26 percent of pregnancies end in miscarriage, many of which require medical intervention to avoid health emergencies such as infection or hemorrhage.[16] Media reports reflect that the unclear language employed by many states in their abortion bans is causing confusion and hesitation among health professionals when handling miscarriages that require medical management, such as the surgical removal of a nonviable fetus and cases in which there is still fetal cardiac activity.[17] This is because treatments for miscarriage are the same as those used to provide an abortion.[18] These reports also demonstrate a growing sense of fear among patients about the care they might receive at health care facilities should they present with common symptoms such as bleeding or pain, as well as anxiety surrounding future pregnancies.
Indeed, prospective patients face the daunting task of trying to determine what these laws mean for the care they can expect to receive in hospitals in states with abortion bans. The answers to these crucial questions may vary considerably across health care institutions. Thus, pregnant people in these states struggle to access necessary information about how their own possible obstetric emergencies might be handled at different hospitals to determine their best options for maternity care, what treatment options are legal, and whether they can receive information in advance to better guide their decision-making.[19] Would a hospital they are considering require multiple layers of bureaucracy to secure approvals to terminate a pregnancy – such as oversight committees or requirements for second physicians to agree that their life is sufficiently at risk – that could create delays, leading to their death? Moreover, can patients trust the hospitals to support clinicians who prioritize their lives in the face of a life-threatening medical emergency? Without receiving clarity on these crucial questions, pregnant people struggle to make informed decisions about where to seek care.
To help answer these questions, Physicians for Human Rights (PHR), Oklahoma Call for Reproductive Justice (OCRJ), and the Center for Reproductive Rights (CRR) have examined Oklahoma as a case study to investigate two key questions:
- Do hospitals in Oklahoma have policies and/or protocols that govern decision-making when pregnant people face medical emergencies, and are pregnant people in Oklahoma able to receive information on these policies, if they do exist?
- If information is provided to prospective patients on hospital policies and/or protocols related to obstetric emergency care, what is the content and quality of that information?
The following report describes the research methodology for this study, its findings, relevant legal and ethical standards, and recommendations based on what the research revealed.
Legal Background
At the time of this writing, Oklahoma has three overlapping abortion bans (two civil and one criminal) in effect as well as a homicide statute that could be applied to the provision of abortion. A fourth ban with criminal penalties was enacted in 2022, but that law was struck down by the Oklahoma Supreme Court in March 2023. These laws have inconsistent prohibitions and penalties, resulting in a dangerous lack of clarity around their application. In particular, the exceptions in the laws permitting abortion in cases of medical emergencies conflict, which has resulted in significant confusion around when abortions are permitted in the face of a medical emergency.
On March 21, 2023, the Oklahoma Supreme Court issued a 5-4 decision upholding the constitutionality of Oklahoma’s 1910 pre-Roe ban on abortion but striking down a 2022 criminal ban on the grounds that its narrow medical exceptions provision violated the “inherent right of a pregnant woman [under the Oklahoma Constitution] to terminate her pregnancy when necessary to preserve her life.” The opinion did not address still-pending challenges to two other civil bans, which both include “medical emergency” language that was found to be unconstitutional in the Court’s decision. The Oklahoma Supreme Court stated that it “would define this inherent right to mean: a woman has an inherent right to choose to terminate her pregnancy if at any point in the pregnancy, the woman’s physician has determined to a reasonable degree of medical certainty or probability that the continuation of the pregnancy will endanger the woman’s life due to the pregnancy itself or due to a medical condition that the woman is either currently suffering from or likely to suffer from during the pregnancy. Absolute certainty is not required; however, mere possibility or speculation is insufficient.” This decision could ultimately provide greater comfort to health care providers treating patients experiencing emergent conditions, but given the other two civil bans still in effect (one of which has the same medical exception deemed insufficient by the Oklahoma Supreme Court), confusion is unlikely to be assuaged at present. At publication, it remains unclear how hospitals will react to the decision.
Legislators have not been able to articulate how these bans operate together. An investigative journalist contacted all 42 lead sponsors and cosponsors of the four recent abortion bans and found that none could “answer basic questions about the bans’ enforcement.”[20] Oklahoma’s attorney general acknowledged confusion about the application of these bans in guidance to law enforcement that was issued on August 31, 2022.[21] The guidance is not binding, and it does not clearly remedy the conflicts, nor does it address the two civil bans.[22]
The four recent abortion bans took effect one after another starting just before the Dobbs decision was released on June 24, 2022. First, Oklahoma enacted two abortion bans modeled after Texas S.B. 8, allowing private citizens to bring lawsuits against those who provide abortions or assist those seeking abortions. Then the state enacted two more abortion bans with criminal penalties. Three remain in effect:
- S.B. 1503 (“6-Week Civil Ban” or “Heartbeat Law,” effective May 3, 2022): The 6-Week Civil Ban prohibits physicians from “knowingly” providing an abortion after “detect[ing] a fetal heartbeat” or if the physician “failed to perform a test to detect a fetal heartbeat.” [23] The law creates a civil enforcement mechanism by which any person not affiliated with the state or local government “may bring a civil action against any person” who performs a prohibited abortion, “knowingly” aids or abets a prohibited abortion, or intends to engage in these activities.[24]
- H.B. 4327 (the “Total Civil Ban,” effective May 25, 2022): The Total Civil Ban shares a similar civil enforcement scheme with the 6-Week Civil Ban, but it applies from the moment of “fertilization.” [25]
- 21 Okla. Stat. § 861 (the “1910 Criminal Ban,” effective June 24, 2022): The 1910 Criminal Ban was an old law blocked after Roe v. Wade was decided, which was revived when “the Attorney General certifie[d] that … [t]he United States Supreme Court … overruled in whole or in part Roe … and … Casey.” [26] Oklahoma’s attorney general issued this certification on June 24, 2022, the same day Dobbs was decided. The statute prohibits an abortion at any point during a pregnancy.[27]
- S.B. 612 (the “2022 Criminal Ban,” struck down by the Oklahoma Supreme Court on March 21, 2023): The 2022 Criminal Ban prohibited abortion at any stage of pregnancy, with more extreme criminal penalties than the 1910 Criminal Ban.[28]
Oklahoma’s homicide statute could also be used to prosecute providers of abortion because the law considers the “killing of an unborn child” to be a homicide, punishable by up to life in prison.[29] Further, medical licensing boards are empowered to discipline clinicians and take action to suspend or revoke their licenses based on any violations of state law.[30]
Oklahoma’s homicide statute could also be used to prosecute providers of abortion because the law considers the “killing of an unborn child” to be a homicide, punishable by up to life in prison.
The resulting statutory framework includes inconsistent definitions, intent provisions, exceptions, and penalties (see table below).
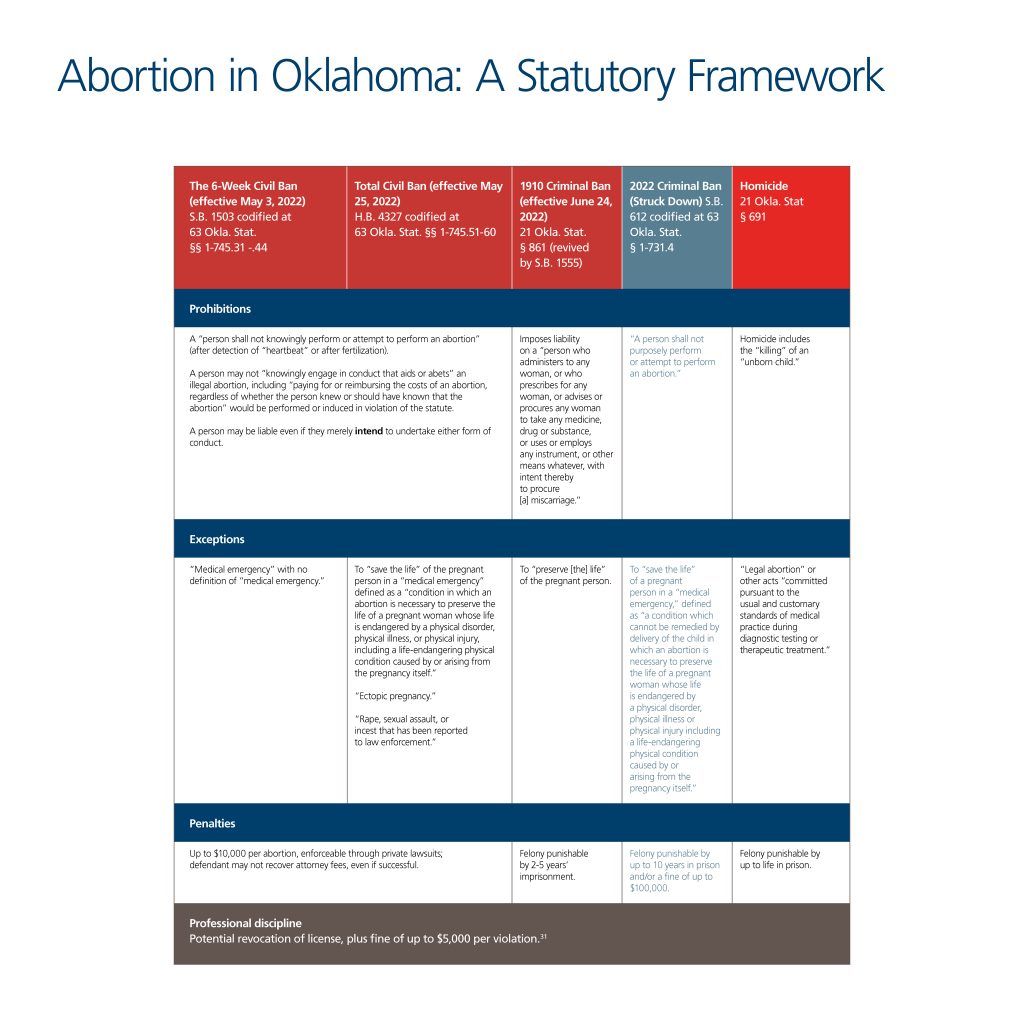
Understanding the scope and nature of permitted exceptions for abortion is particularly challenging under these laws. The Total Civil Ban permits abortion only when necessary to preserve a person’s “life in a medical emergency,” defined as a “condition in which an abortion is necessary to preserve the life of a pregnant woman whose life is endangered by a physical disorder, physical illness, or physical injury, including a life-endangering physical condition caused by or arising from the pregnancy itself,” although the 2022 Criminal Ban was struck down because of an almost identical “medical emergency” exception.[32]
The other abortion bans in effect, however, do not discuss exceptions based on specific medical emergencies. The 6-Week Civil Ban contains an exception for medical emergencies but does not define what counts as a medical emergency.[33] The 1910 Ban, which has now been upheld by the Oklahoma Supreme Court, similarly includes no mention of specific medical emergencies, as it only permits abortions to “preserve [the] life” of the pregnant person.[34] Meanwhile, Oklahoma’s homicide statute criminalizes the killing of an “unborn child,” except for a “legal abortion” or other acts “committed pursuant to the usual and customary standards of medical practice during diagnostic testing or therapeutic treatment.”[35] Further, the Total Civil Ban explicitly exempts care for an “ectopic pregnancy” and allows abortion for pregnancies resulting from “rape, sexual assault, or incest that has been reported to law enforcement.”[36] None of the other bans expressly carves out such exemptions.
Under these provisions, physicians cannot know when they are legally permitted to end a pregnancy. In a “medical emergency” that merely “endangers” the life of the patient, must they wait until the patient’s life is in immediate jeopardy? What criteria must be used to determine that this threshold is met? For example, are ectopic pregnancies (a dangerous medical condition in which a fertilized egg implants outside of the uterine cavity, typically in a fallopian tube) clearly exempted? The Oklahoma bans fail to answer these vital questions.

Impacts on Health
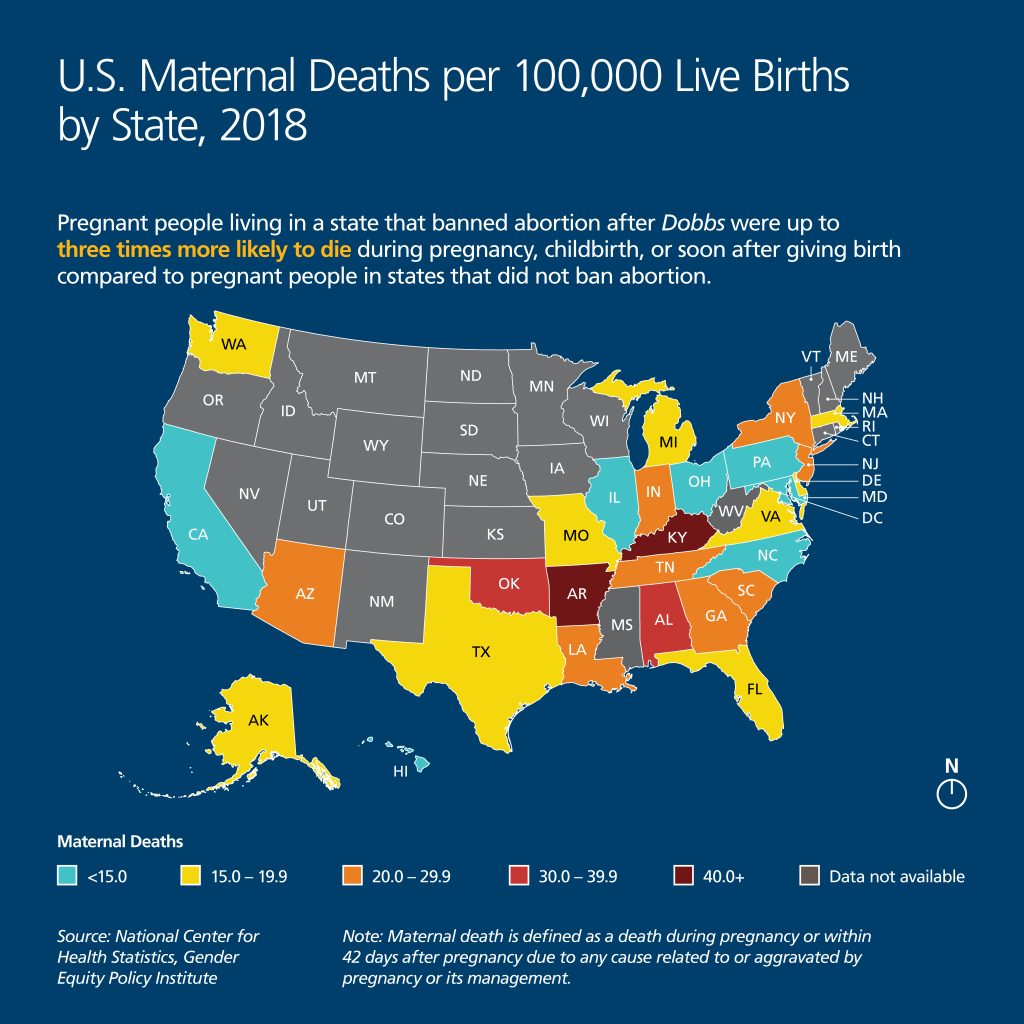
The medical literature is clear that criminal abortion bans are linked to a range of negative physical and mental health outcomes for pregnant people, in the United States and around the world. The unworkability of even an exception in the context of medical emergencies particularly implicates maternal mortality and morbidity. Constraining physicians from providing necessary care in medical emergencies is extremely dangerous for patients. The United States already has the highest maternal mortality rate of all high-income countries, with the U.S. maternal death rate further increasing over the COVID-19 pandemic, from 20.1 deaths per 100,000 live births in 2019, to 23.8 in 2020, to 32.9 in 2021.[37] Moreover, “For every U.S. woman who dies as a consequence of pregnancy or childbirth, up to 70 suffer hemorrhages, organ failure or other significant complications, amounting to more than 1 percent of all births,” according to data from ProPublica and NPR.[38] This crisis in U.S. maternal health outcomes disproportionately impacts people from Black, Indigenous, and low-income communities, who consistently face the greatest risks during their prenatal, pregnancy, childbirth, and postpartum phases linked to historic discrimination and inadequate access to quality health care. [39]
The medical literature is clear that criminal abortion bans are linked to a range of negative physical and mental health outcomes for pregnant people, in the United States and around the world. Constraining physicians from providing necessary care in medical emergencies is extremely dangerous for patients.

According to the Gender Equity Policy Institute, pregnant people living in a state that banned abortion after Dobbs were up to three times more likely to die during pregnancy, childbirth, or soon after giving birth compared to pregnant people in states that did not ban abortion.[40] This continues a trend in the United States wherein states that support reproductive health services, including by expanding Medicaid and supporting access to abortion and contraception, have lower maternal mortality rates than states that have restricted access to reproductive health care.[41] These disparities will likely increase as abortion bans continue to take effect around the country, with people of color among the most likely to suffer.[42]
Oklahoma exemplifies this alarming trend. Black and Indigenous residents of Oklahoma face significantly higher rates of maternal mortality than white residents. Moreover, Oklahoma “persistently ranks among the states with the worst rates” of maternal deaths in the United States, and maternal deaths in Oklahoma have “increased in recent years.”[43] According to the Oklahoma State Department of Health, from 2004 to 2018, Black pregnant women in Oklahoma suffered “more than 2.5 times the rate of deaths compared to the white population,” a statistic the Oklahoma Maternal Mortality Review Committee called an “alarming disparity.”[44] The Department further concluded that Indigenous pregnant women in Oklahoma “have experienced up to 1.5 times the rate of deaths when compared to white women over the years.”[45]
According to the Gender Equity Policy Institute, pregnant people living in a state that banned abortion after Dobbs were up to three times more likely to die during pregnancy, childbirth, or soon after giving birth compared to pregnant people in states that did not ban abortion.
Methodology
The findings of this report are based on a “simulated patient” research methodology, in which research assistants posed as prospective patients and called hospitals that provide prenatal and peripartum care across the state of Oklahoma to ask questions related to emergency pregnancy care.[46] The value of this methodology is its ability to elicit realistic responses from staff, akin to how they would behave when dealing with an actual patient, thus avoiding the social desirability biases associated with self-reporting.[47] These methods have been used successfully in multiple studies of hospital practices and have been deemed scientifically and ethically sound.[48] This study was reviewed and deemed exempt from U.S. requirements for human subjects research by Physicians for Human Rights’ (PHR’s) Ethics Review Board (ERB).[49]
Two PHR research interns and one staff member were trained and used a standard script to call all hospitals in the state listed as offering labor and delivery services. Presenting themselves as prospective maternity patients choosing which hospital to go to for prenatal and peripartum care, they requested information about each hospital’s policies and procedures that would guide decision-making in: 1) cases of medical emergencies, where their life could be at risk if a pregnancy with a viable fetus were not terminated; and 2) cases of miscarriage that require procedures both when there is and when there is not fetal cardiac activity.
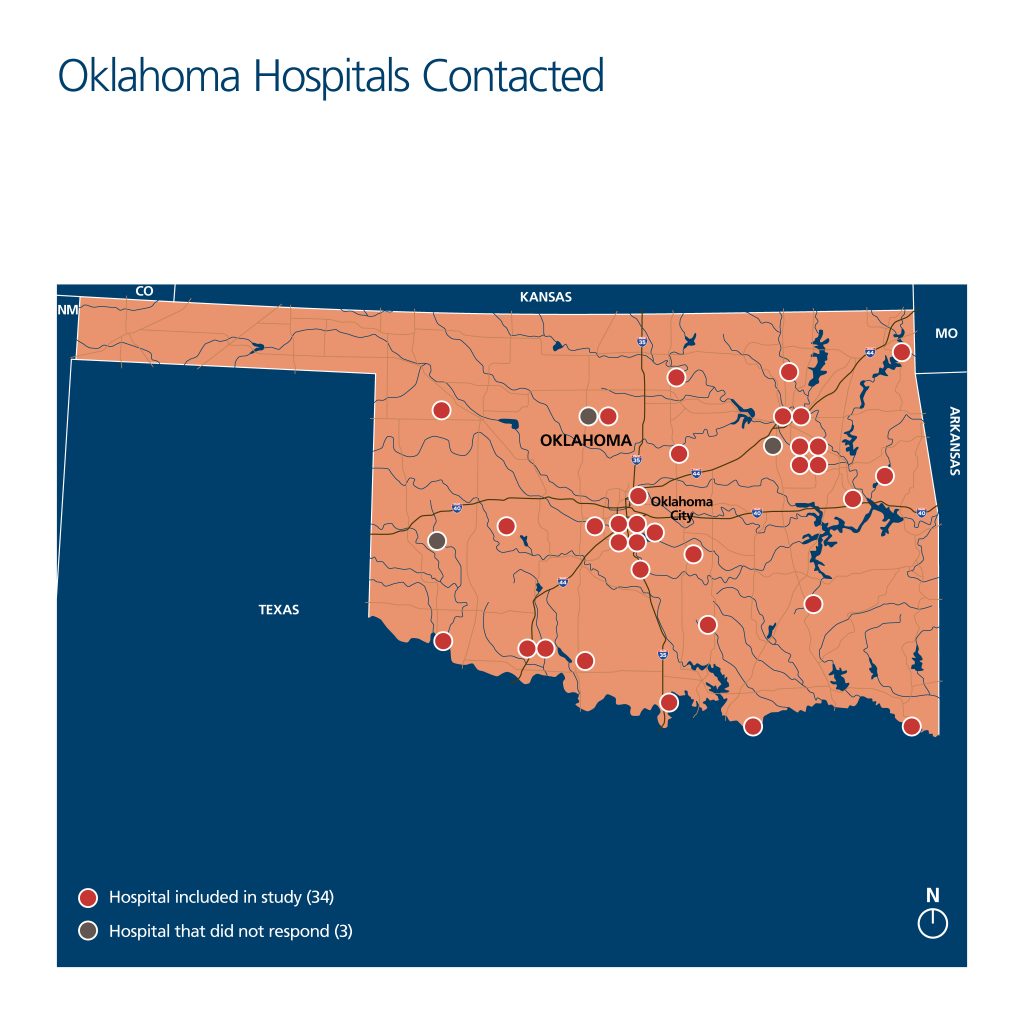
To identify hospitals to be called, the research team reviewed several databases of all registered hospitals in Oklahoma maintained by the Oklahoma Hospital Association and by OfficialUSA.com.[50] The team then examined each hospital’s website to identify facilities that offer prenatal and peripartum services. In obstetric emergencies, hospitals’ obstetrics and labor and delivery clinical teams and departments are typically where difficult decisions about what constitutes “medically necessary” abortions are made and where such procedures are eventually carried out. From the review of each hospital’s website, the research team identified 41 facilities providing labor and delivery services in Oklahoma.
Since a prospective patient would likely first seek information from hospital websites, staff reviewed each hospital’s website in October 2022 for information on care in cases of potential miscarriage and medical emergencies during pregnancy. Two hospital websites described surgical procedures to remove ectopic pregnancies. No hospital website discussed care provided in other cases of medical emergency that could threaten the pregnant person’s life, and no hospital website described possible procedures or other treatment in cases of a potential miscarriage.
Staff members then built profiles for each of the 41 identified hospitals, categorizing them according to their religious affiliation, academic affiliation, size, association with an Indigenous nation, and geography. The four identified hospitals affiliated with an Indigenous nation were not included in the calls because it is currently unclear what the legal effects of Oklahoma’s bans are within these facilities, given that the Indian Health Service, which operates them, is under federal rather than state oversight (these facilities are also affected by the Hyde Amendment).[51] Thus, a total of 37 hospitals were called during the months of November and December 2022.

The simulated patients were assigned specific regions of the state to call (east, north, central, south, west), with a greater distribution of hospitals in Oklahoma’s central and northeastern regions. Each was trained to use a caller script and standardized note-taking sheet but was encouraged to alter the language and cadence of the questions, in the interest of appearing as realistic as possible and as individual conversations warranted. Each caller introduced herself under the following identity: a 36-year-old, highly educated, affluent, married woman with mild pre-existing conditions who had recently moved to Oklahoma.[55] The researchers stated that this was their first pregnancy and that they were currently six weeks pregnant. Callers used their real first names and a fictional last name in conversations and were provided an email address and the name of a universally accepted insurance plan (Blue Preferred PPO) to give hospital staffers if requested. If asked about their ethnicity, the research assistants were instructed to give their real backgrounds; all three callers were white women. Lastly, if callers were asked about their place of residence, all explained that they lived near the hospital called.
Written notes from the calls were kept on a standardized form. When relevant, the researchers wrote down verbatim quotes from hospital staff; however, none of the calls were recorded. Personal cell phones were used to make all calls.
During the calls, simulated patients requested to be informed about hospital policies that guided decision-making processes for “medically necessary” abortions to save the life of a pregnant patient and about the internal approval processes, if any, for conducting these procedures. The caller initially asked general questions about the hospital facility, such as if the hospital offered private delivery rooms, before shifting to more specific questions about the hospital’s guidelines in cases where an abortion might be required to save the life of the pregnant patient. As a pregnant person who recently moved to Oklahoma with her spouse, each caller’s questions were meant to convey a relatively informed patient’s concerns about how state-level abortion bans might affect the care they would receive in the case of a medical emergency, particularly given the existence of pre-existing, if routine, conditions.
In all calls, the simulated prospective patients requested to be connected to a qualified hospital representative who could answer their questions about care options during pregnancy. When hospital staffers provided vague or unclear explanations of hospital policies, callers gently probed for further clarification and, when necessary, requested to speak to another hospital employee who might have more complete information. If their efforts to speak to someone knowledgeable about hospital policies were unsuccessful during the call, the caller would thank the staff member, hang up, and call again later. Calls were considered complete if the callers were able to receive an answer about hospital policies or lack thereof from a member of the staff. If the initial call was inconclusive, the researchers would call hospitals back up to two more times before concluding the case. When a hospital provided information about its policies and guidelines for clinicians (or the lack thereof), verbally or through written communication, this was considered a “complete” call, and the call sheet was finalized. As discussed below, researchers were able to conduct “complete” calls with 34 Oklahoma hospitals.
Each completed call lasted approximately 15 minutes, with all efforts made to minimize call time so as not to burden hospital staff. If the hospital offered to set up an in-person or virtual appointment, the caller would decline the offer. All notes taken by the callers were de-identified and were stored on a password-protected server, accessed only by study staff associated with PHR. Hospitals were anonymized in these documents and for the report, using internally designated hospital IDs.
Of the 37 hospitals called, the callers reached staff who were able to talk about their policies at 34 facilities (92 percent response rate). At three hospitals, callers were transferred to appropriate representatives who never picked up, even after multiple attempts. There were no common characteristics among these three hospitals. For this reason, the universe of data for this report is the 34 Oklahoma hospitals where researchers were able to conduct a “complete” call.
At 23 hospitals (68 percent), the caller’s questions about hospital policies were answered in the first phone call. However, second or third calls were sometimes required because calls were dropped unexpectedly, staff did not initially answer the phone, or the callers had not received clear or conclusive answers in the first attempt. The callers were able to receive answers from eight hospitals (23 percent) after the second call and three (nine percent) after the third call. At all hospitals, the callers were referred to the labor and delivery unit/department or its equivalent. At six hospitals (approximately 18 percent), the callers spoke directly with a nurse.
Limitations
Four limitations to the “simulated patient” methodology and research design are worth noting. First, to the extent that any hospital staff members doubted the simulated callers’ identities, the responses they gave may have been incomplete or otherwise failed to disclose relevant information. There was no indication that hospital staff had such doubts, but it is a possibility.
Second, interactions with frontline staff and clinicians in these calls may or may not accurately reflect internal hospital policies or procedures, as this would depend upon the specific knowledge of the individual(s) spoken to. For all completed calls, the callers always spoke directly with labor and delivery ward staff members, while at six hospitals they were referred to speak directly with nurses, and at several others, hospital staff consulted clinicians. Definitive conclusions therefore cannot be drawn about whether hospitals did in fact have policies and guidelines, nor about what the content of any such policies and guidelines might be. However, because the aim of the study was to assess whether a prospective patient could receive necessary information to help guide an informed decision about where to receive maternity care, the information gained by the callers, whether accurate or not, is representative of what prospective patients would likely receive if they sought this information themselves.
Third, the callers’ fictional profiles are not representative of people who stand to be most harmed by Oklahoma’s abortion bans: low-income people, Black and Indigenous people, and other people of color. According to the standard script, the callers held universally accepted insurance plans, demonstrated that they were well-informed about Oklahoma’s anti-abortion laws, and in many cases were quite assertive in seeking to receive answers to their questions, insisting on speaking to other hospital staff if the initial person answering the call did not know whether there were hospital policies relevant to the inquiries. The study, therefore, does not assess what responses hospitals would give to those who do not have health insurance (currently an estimated 16 percent of adults in Oklahoma), who have less comprehensive or widely accepted insurance plans and thus lack the option of seeking care at another hospital, who are less empowered or assertive, who have lower health or English literacy, or who are unaware of Oklahoma’s abortion laws.[56] Moreover, although they did not identify themselves by race or gender identity, the caller-researchers were cisgender white women. They therefore do not share the lived experience of those who face discrimination and other barriers in accessing health care and experience significant disparities in maternal health outcomes, including Black and Indigenous people or other people of color, gender-nonconforming or transgender people, migrants, and those with low health or English literacy.
Finally, because hospitals serving Indigenous populations were not included in the study, conclusions cannot be drawn about prospective patients’ ability to receive information from these hospitals about their internal policies. This is an important limitation, as Oklahoma’s Indigenous population, which constitutes almost 10 percent of the state’s total population, has disproportionately worse maternal, infant, and child health outcomes than white Oklahomans. Given these disparities, it will be important to closely monitor the post-Dobbs maternal mortality and morbidity outcomes for Indigenous communities.
Notwithstanding these limitations, the results are meaningful. The fictional profile of the callers served the intended purpose of the study. That profile was chosen to ensure that results reflect the highest level of transparency a hospital would offer to prospective patients who request information to help determine where – among multiple options available to them – they would like to receive maternity care.
Overview of Findings
Staff members at most hospitals contacted demonstrated a willingness to talk with the simulated prospective patients about their concerns and sought to reassure the callers that they would still receive a high level of care under the new abortion laws. However, not a single hospital appeared to be able to articulate clear, consistent policies for emergency obstetric care that supported their clinicians’ ability to make decisions based solely on their clinical judgement and pregnant patients’ stated preferences and needs. At most hospitals, representatives were unable to tell the callers whether there was an approval process or any other guidelines to help clinicians determine that a pregnancy must be terminated to save the life of the patient, and they were similarly unable to describe what miscarriage management services were available to patients. In a few outlier cases, representatives explained that their hospitals had instituted such policies but refused to provide this information, in some cases citing an inability to share material with those outside of the hospital system, and in others offering no explanation. And in several hospitals, different representatives provided contradictory information about hospital policies and/or incorrect information about Oklahoma’s abortion laws.
Not a single hospital appeared to be able to articulate clear, consistent policies for emergency obstetric care that supported their clinicians’ ability to make decisions based solely on their clinical judgement and pregnant patients’ stated preferences and needs.
Callers received confusing and at times conflicting information about what would constitute a medical emergency and who could decide whether the emergency warranted terminating a pregnancy. Most hospitals reported that it is up to the treating doctors to make determinations about what constitutes a medical emergency where the pregnant person’s life is at risk. It was not clear, however, whether physicians are given guidance and legal support, nor whether they are required to complete certain procedures when they determine that a medical emergency exists that necessitates terminating a viable pregnancy. One hospital representative’s response exemplified the lack of clarity and transparency during the calls by claiming, “If the situation is truly life-threatening, decisions will be made,” without explaining what qualifies as “life-threatening,” how those decisions would be made, or by whom. At several hospitals, representatives explained that if a physician diagnoses a patient as experiencing a medical emergency that places the patient’s life at risk and requires an abortion, the physician must wait to receive approval from other entities – such as an ethics committee or a second physician – before terminating the pregnancy, raising concerns about the risk of possible harmful or even fatal delays.
The callers also received little clarity about how hospital administrations advise medical personnel to prioritize patient input, safety, and medical ethics during medical emergencies. In calls with most hospitals, no assurance was provided that the simulated patient would have a role in decision-making about pregnancy termination in medical emergencies where their life could be at risk. At one hospital, the caller was told, “You get a voice, but doctors make the final decision.” Moreover, at most hospitals, the callers were not provided reassurance that the pregnant patient’s life would be prioritized in medical decision-making. One hospital representative assured the caller that, “Here, we care equally about both the mother and the fetus” but did not answer further questions about which would receive priority if a choice of one or the other had to be made.
One hospital representative’s response exemplified the lack of clarity and transparency during the calls by claiming, “If the situation is truly life-threatening, decisions will be made,” without explaining what qualifies as “life-threatening,” how those decisions would be made, or by whom.
Finally, miscarriage management procedures previously available to patients appeared to have been restricted in some hospitals after the passage of recent abortion laws in Oklahoma. For example, several hospitals cited the new “heartbeat law” (S.B. 1503) as the reason why they no longer perform procedures in cases of miscarriage. At seven hospitals, representatives avoided answering questions about cases in which the life of a patient with a viable pregnancy would be at risk. At one hospital, for example, the nurse repeatedly shifted the discussion to cases in which “there is no fetal heartbeat.” In those cases, the nurse stated, “When we have a situation where a baby no longer has a heartbeat, that’s between the physician and patient how to move forward.”
The study’s findings demonstrate that despite apparently good-faith efforts from most hospital representatives, callers could access little information, and the information they received was often conflicting and confusing – at some hospitals, callers received contradictory information from separate staff within the same hospital. These findings raise grave concerns about the ability of a pregnant person in Oklahoma – and other states with similar abortion bans – to receive clear, sufficient, and necessary information to make informed decisions about their medical care, and the ability of such patients to receive medically-necessary treatment. Callers also found that some hospital administrations, in an effort to comply with state laws, imposed restrictive policies on medical personnel that would impede their ability to provide prompt and effective care for pregnant patients.
At most hospitals, the callers were not provided reassurance that the pregnant patient’s life would be prioritized in medical decision-making.
1. Staff at Most Hospitals Provided No Information or Conflicting Information on Hospital Policies or Guidelines for Clinical Decision-Making in Medical Emergencies
At the start of every call, the callers asked hospital staff, “What are your hospital’s procedures if I were to face a medical emergency while pregnant that jeopardizes my life?” In response, staff at 22 hospitals (65 percent) were unable to provide information about procedures, policies, or support provided to doctors during medical emergencies when the clinical decision was that it was necessary to terminate a pregnancy to save the life of a pregnant patient. Staff at eight hospitals recommended that callers set up appointments with a doctor affiliated with the hospital, to ask them directly how they would approach medical emergencies and to discuss specific health concerns. In some cases, the callers were assured that through these appointments, they could learn more about each doctor’s views on these issues to help them select their preferred provider. However, when patients have an emergency, they are unlikely to be able to ensure that they receive care from a preferred provider.
Three hospitals stated that they were aware of internal policies but that they were not willing to share specific procedural information with the callers. Of these three:
- One hospital told the caller that she could not receive additional information about hospital guidelines for doctors until she was a patient at the hospital.
- Another hospital representative stated that guidelines are for internal use only and are not shared with patients.
- One representative offered to email the hospital’s written policies for handling emergency pregnancy situations, with the approval of her supervisor. However, although the caller left her email address with the staff member and contacted the hospital to confirm that they were sending the written policies, the information was never sent.
These findings raise grave concerns about the ability of a pregnant person in Oklahoma – and other states with similar abortion bans – to receive clear, sufficient, and necessary information to make informed decisions about their medical care, and the ability of such patients to receive medically-necessary treatment.
The callers were able to talk directly with nurses at six hospitals (approximately 18 percent). However, the information the clinicians provided was often no clearer than that provided by other hospital representatives. Although clinicians initially provided more information about the approval process required to terminate a pregnancy at their hospital (five of six nurses), compared to labor and delivery receptionists (13 of 28 receptionists), their seemingly greater knowledge about hospital policies was undercut by a tendency to provide incorrect information or to advise receptionists and other staff to withhold information from the callers. Some receptionists put callers on hold to consult with nurses or physicians and, upon their return, told the callers that they had been advised not to answer any questions about hospital policies. For instance:
- After consulting with a nurse, one hospital representative merely repeated in response to each of the caller’s questions, “I cannot advise on that.”
- At another hospital, a staff member who consulted with a physician returned to the call and reported (incorrectly) that “Nowhere in the state of Oklahoma can you get an abortion for any reason.”
In such cases, callers’ inability to access information could not be attributed to failure to reach medical experts; rather, clinicians did not provide accurate or meaningful information to the callers.
In two of the 11 hospitals in which callers spoke with multiple hospital representatives during a call, the callers received conflicting accounts of internal policies. At one hospital, two different staff members with whom the caller spoke provided contradictory information about the role of an ethics committee in decision-making during medical emergencies. Within the same call, one representative claimed that doctors would need the approval of an ethics committee to “sign off” on all determinations that a pregnancy needed to be terminated to save the life of the pregnant patient, whereas another stated that the committee is only required to sign off when patients are incapacitated and unable to communicate their preferences to a doctor.
Similarly, hospital staff conveyed a lack of knowledge and provided incorrect information about state laws affecting emergency pregnancy care in Oklahoma. For instance:
- Of the nine cases (27 percent) in which hospital representatives explicitly discussed the Oklahoma abortion bans, three explained that they did not know how recent laws would change the types of care hospitals can provide.
- One hospital representative asserted that ending a pregnancy as a treatment for a medical emergency “do[es] not count” as an abortion procedure under state law.
In calls with two hospitals, staff revealed that there were disagreements and discontent among medical professionals in their facilities about their hospitals’ responses to the new abortion bans. In one call, a nurse noted that there was a difference of opinion among physicians at their facility on how to act in emergency pregnancy situations, as well as on what constitutes an “emergency.” Similarly, a staff member at another hospital noted that not all nursing staff were “on board” with how their hospital had been providing care since the new state abortion laws.
At 10 hospitals, most of which were smaller and in non-urban areas, staff explained that patients would be transferred to another hospital if complications arose because their facility lacked the capacity to handle high-risk cases. But in none of those instances could the representative convey information on the policies of the facility to which they would be sending patients.
In sum, hospital representatives frequently demonstrated confusion, uncertainty, and lack of knowledge about the state of emergency obstetric care in the wake of Dobbs. No representatives were able or willing to share internal written policies with patients, even in cases where they indicated knowledge that their hospitals had such policies. And in those instances where clinicians were consulted, they often provided conflicting and incorrect information about hospital policies and state laws.
Hospital representatives frequently demonstrated confusion, uncertainty, and lack of knowledge about the state of emergency obstetric care in the wake of Dobbs.
It is important to note that at almost all the hospitals reached, staff responded to the callers in an empathetic manner and sought to reassure them about their commitment to patient safety and well-being. A staff member at one hospital reassured the caller of their extensive track record of handling similar cases, claiming that “we are the highest high-risk hospital in Oklahoma.”
Staff members at seven hospitals (21 percent) assured the callers that the safety of the pregnant patient is of paramount importance to medical personnel.
- At one hospital, a staff member emphasized that, “We want to take care of the mom and baby, but we’ll have to take care of you first.”
- In another case, the caller was reassured that, “You don’t need to be on the edge of dying before doctors act.”
- Some hospital staff explicitly expressed sympathy for the callers’ worries, explaining that they “completely understand” why callers were concerned following recent abortion bans and noting that their questions were “good questions to ask.”
Even at hospitals where staff sought to reassure the callers, however, they were not able to provide information on hospital policies that would back up their assurances. Indeed, one representative seemed to recognize the dual loyalty predicament clinicians now face in Oklahoma, stating that, “It is tricky because of state laws, but we will not let the mom die.”
At one hospital, a staff member emphasized that, “We want to take care of the mom and baby, but we’ll have to take care of you first.” In another case, the caller was reassured that, “You don’t need to be on the edge of dying before doctors act.”
2. It Was Unclear What Criteria Clinicians Use in Determining When Pregnancies Can Be Legally Terminated
Few hospital representatives could provide clear answers to the callers about what criteria doctors might use to determine which medical conditions would classify as medical emergencies that threaten the pregnant person’s life, and, as a result, might warrant performing an abortion. While all patient care must be tailored to the condition and needs of the individual patient, individual clinicians may struggle to determine what level of danger to a patient’s health is legally required in order to permit an abortion, in addition to having differing views about medical necessity. As noted by one receptionist, “Not all doctors agree with each other on how emergency decisions are made and what emergency care should look like.” Representatives at seven hospitals (21 percent) shared examples of criteria that might be used to determine whether a life-threatening medical emergency exists. These included assessing the amount of vaginal bleeding (three hospitals), if the patient presents with a uterine infection or is septic (i.e., has a systemic, life-threatening infection) (two hospitals), or if they present with an ectopic pregnancy (two hospitals).
At one hospital, the representative both mischaracterized procedures to remove ectopic pregnancies as “abortions” and incorrectly described them as the only type of medical emergency that would meet Oklahoma’s legal criteria of saving the life of the pregnant person. She asserted that only ectopic pregnancies would count as medical emergencies that justify “abortion procedures,” drawing a false equivalence between ectopic pregnancies and other conditions that might warrant an abortion.[57]
The simulated patients also received little information about the guidance and support clinicians receive when deciding whether to terminate a pregnancy. Representatives at 16 hospitals (47 percent) suggested that doctors make decisions in such cases but did not provide any information about institutional guidance or support given to clinicians when they determine that a pregnancy should be terminated. Two hospital representatives noted that doctors receive legal counsel when they determine that a pregnancy needs to be terminated to save the life of the pregnant patient.
- In one instance, the caller was told that, in some cases, the hospital’s legal advisors and ethics board are consulted, but when they become involved “depends on the situation.”
- In the other instance, a hospital representative claimed that where the pregnant person’s life is possibly in danger and there is still a “fetal heartbeat,” medical staff would consult the legal team, but would still “not let the mother die.”
It is unclear from the information provided what role the legal counsel serves in these two hospitals. As a formal legal team defending against criminal or civil penalties, counsel could constitute a helpful support system for clinicians. However, internal policies that require legal counsel to sign off before physicians can terminate a pregnancy create procedural barriers that can delay necessary care and place pregnant patients at risk.
At three hospitals (nine percent), representatives stated that, although they would not perform “abortion procedures,” they would handle medical emergencies where the pregnant person’s life is in danger by inducing labor and delivering the fetus vaginally or with a cesarean section. Another three hospital representatives explained that they were uncertain about how new state laws would affect what procedures they can provide, and whether these would render previously acceptable procedures illegal.
3. In a Majority of Cases, Callers Received No Clear Information About Whether Internal Administrative Oversight Mechanisms Were Required to Provide Approval in Cases of Medical Emergencies
At four hospitals, representatives reported that a committee or another authority figure is required to sign off before the hospital can provide medically necessary abortions. These mechanisms include gaining approval from an ethics board (three hospitals) or a second doctor (one hospital). In one of these cases, the representative sought to reassure the caller that, although they required approval from an oversight committee, they would not let the patient die.
In another 14 cases (41 percent), hospital representatives provided unclear and/or incomplete answers about whether doctors require approval to perform a medically necessary abortion. One representative, for example, claimed that doctors at that hospital are not allowed to perform certain procedures for “ethical reasons,” but would not clarify what those procedures or ethical concerns are. It was unclear whether this representative meant that doctors require the approval of an internal ethics board, or that doctors should follow ethical guidelines created by national medical bodies such as the American College of Obstetricians and Gynecologists (ACOG). Many of these representatives also did not directly answer whether doctors were required to receive hospital approval to perform abortions, leaving the callers uncertain about hospital policy. In one case, the representative avoided answering the question by only discussing circumstances where the “fetus has no heartbeat.”

4. Hospital Staff Rarely Talked About Prioritizing Patient Safety, Patients’ Role in Making Decisions in Medical Emergencies, or Professional Ethics
The callers received little clarity about how patient input and safety would be prioritized during medical or obstetric emergencies. Staff members at 27 hospitals (79 percent) either did not offer information about patients’ roles in decision-making or, in one case, stated that, “You get a voice, but doctors make the final decision.” In two cases, patients were told that medical decisions “also depend on what your husband and family want.”
Hospital representatives at only seven hospitals (21 percent) affirmed to the callers that they would have a role in deciding whether to terminate a pregnancy in obstetric emergencies when their life could be at risk. For example:
- A staff member at one hospital stated, “It is entirely your decision how the doctors take care of you,” adding that they require the patient’s consent before performing any care.
- A representative at another hospital stated that patients can request a second opinion or involve the ethics review board if they disagree with the decision reached by their doctor about terminating a pregnancy in medical emergencies.
In the same vein, the callers received inconsistent and varied messaging about doctors’ priorities when treating medical emergencies in pregnant patients.
- Representatives at only seven hospitals (20 percent) voluntarily shared that their hospitals prioritize the life of the pregnant person. In two cases, hospital representatives explained that “We want to take care of the mom and baby but we’ll have to take care of you first,” and that the hospital staff would do “anything necessary to save [your] life because that is the [hospital name]’s way.”
- At six hospitals (18 percent), hospital representatives stated that, at their facility, the life of the pregnant person and fetus are prioritized equally.
- At one hospital, representatives suggested that during an emergency, medical personnel would use the pregnant person’s body as an “incubator” to carry the baby as long as possible.
Representatives at 21 hospitals (62 percent) offered no information on how staff prioritize saving the fetus over saving the life of the pregnant person in medical emergencies.
Finally, it was unclear to the callers whether hospital staff were aware of or actively considering how medical ethics and professional responsibilities affect the type of care provided to pregnant patients. Only two hospital representatives, for instance, noted that doctors follow the guidance of national medical associations such as ACOG.[58] Instead, most representatives never mentioned ACOG guidelines or any other relevant obligations, nor could they clearly define, when asked, the guidance that informed medical decision-making relating to abortion. One discussion about ethics and hospital responsibilities focused on the hospitals’ religious affiliation. In this case, hospital staff explained that their Catholic background meant that the administration already had rules similar to those in the recent abortion bans.
Representatives at only seven hospitals (20 percent) voluntarily shared that their hospitals prioritize the life of the pregnant person. At one hospital, representatives suggested that during an emergency, medical personnel would use the pregnant person’s body as an “incubator” to carry the baby as long as possible.
5. There Was Significant Variability among Hospitals about How Miscarriages Would Reportedly Be Handled, Especially Where There Was Still Fetal Cardiac Activity
When asked about the types of miscarriage management services offered, representatives at most of the hospitals reported that physicians were able to perform a wide range of treatment procedures in cases where there was no fetal cardiac activity. In the words of one nurse, “When we have a situation where a baby no longer has a heartbeat, that’s between the physician and patient how to move forward.” Representatives at 25 hospitals (74 percent) stated that dilation and curettage (D&C) and dilation and evacuation (D&E) – both techniques to remove fetal, placental, or uterine tissue after an incomplete or threatened miscarriage or as part of an abortion – are allowed at their hospitals when there is no detected fetal cardiac activity. Representatives at two hospitals avoided commenting on using D&C procedures to remove fetal tissue by only discussing placental tissue. The representative at one hospital stated categorically that their hospital prohibits D&E and D&C procedures after 16 weeks of pregnancy, even though many miscarriages occur after that point.
However, in situations where medical personnel detect fetal cardiac activity, few representatives were able to state that their hospital provides miscarriage management services necessary to protect the life of a patient. Five hospitals (15 percent) explained that, because of the “heartbeat law” passed in the state, doctors are not allowed to end a pregnancy when fetal activity is detected, regardless of the viability of the fetus. Seventeen hospitals (50 percent) explicitly told patients that D&C and D&E procedures are allowed during obstetric emergencies if there is detected activity, a third fewer than those who reported allowing these procedures in cases of no detected fetal cardiac activity. Geographically, the hospitals willing to perform D&C and D&E procedures in cases of fetal cardiac activity were primarily clustered in urban centers in the northern and central regions of Oklahoma. Of the 17 hospitals that allow D&C and D&E procedures in cases of fetal cardiac activity, two also imposed additional requirements: one obligated doctors to receive approval from a legal counsel, and the other stated that doctors must “exhaust other options” before performing the procedure.
These findings demonstrate the pernicious impact of Oklahoma’s laws on pregnant patients who are seeking to understand policies and procedures that might guide medical decision-making should they experience a medical emergency. They suggest that pregnant people in Oklahoma, and likely those in the other 12 states with similar laws, face significant obstacles and may be unable to receive necessary information to guide their decisions on where to receive obstetric care. The high frequency of inconsistent, incomplete, and unclear information the simulated callers received is alarming and suggests that hospitals in Oklahoma are struggling to articulate their response to obstetric emergencies in light of the state’s new abortion laws. Taken together, the study’s findings raise serious concerns about the impact of Oklahoma’s anti-abortion laws on patients’ right to information concerning their sexual and reproductive health and their right to receive appropriate, evidence-based care.
The study’s findings raise serious concerns about the impact of Oklahoma’s anti-abortion laws on patients’ right to information concerning their sexual and reproductive health and their right to receive appropriate, evidence-based care.
Legal and Ethical Standards
This case study focuses on the challenges that pregnant people face in getting information on how abortion bans in Oklahoma will affect their ability to receive life-saving care in the case of medical emergencies. That question further unfolds in a context in which hospitals themselves are struggling to navigate these laws, share clear information with prospective patients, and continue providing care that conforms with medical ethics. The inability of the hospitals called in this study to provide clear and accurate information about the care pregnant patients would receive if facing a pregnancy-related medical emergency at any given institution is a reflection of the untenable situation hospitals face under the current abortion bans.
The section below outlines how Oklahoma’s laws – and others like it – conflict with and depart from international human rights law and from the ethical guidelines issued by a range of professional medical associations.
Obligations under International Human Rights Law
International human rights law protects people’s access to reproductive health care and the exercise of reproductive decision-making.[59] Over the past 25 years, the international community has clarified that abortion is a fundamental human right, and jurisprudence from international human rights bodies establishes that access to abortion is necessary to protect the rights to health, life, non-discrimination, information, privacy, and freedom from ill-treatment, harmful practices, and gender-based violence.[60] In March 2022, the World Health Organization (WHO), the leading global public health expert body, published an updated Abortion Care Guideline, which recognizes abortion as an essential health service that is necessary for the realization of human rights.[61]
International human rights law protects people’s access to reproductive health care and the exercise of reproductive decision-making. Over the past 25 years, the international community has clarified that abortion is a fundamental human right.
Abortion access is essential to the right to health, which includes the right to reproductive and sexual health.[62] Accordingly, United Nations (UN) human rights treaty monitoring bodies have established that abortion, like other reproductive health care, must be available, accessible (including affordable), acceptable, and of good quality.[63] States (referring to government at all levels) must provide abortion services and information to all people who may require them.[64] In addition, pursuant to the right to health, states must address the underlying social determinants of health, which are comprised of the social, economic, and cultural factors that can determine an individual’s health.[65]
Abortion access is also critical to the right to life. UN human rights bodies have long recognized and reinforced the WHO’s findings that restrictive abortion laws lead to high rates of unsafe abortions and attendant maternal mortality and morbidity.[66] And they have repeatedly ruled that states should protect people from the physical and mental health risks associated with unsafe abortions.[67] Consistent with this recognition, the UN Human Rights Committee, which is charged with overseeing interpretation and implementation of the International Covenant on Civil and Political Rights, a treaty ratified by the United States, has confirmed that the right to life contains important protections for access to abortion. It limits the restrictions that states can place on abortion access and obligates governments to ensure access to abortion, at a minimum where a person’s life and health are at risk, or when carrying a pregnancy to term would cause substantial pain or suffering.[68] Other treaty bodies have likewise found that access to safe and legal abortion is essential to reproductive health and a prerequisite to safeguarding the right to life, among other rights.[69]
Accurate information about abortion care is likewise critical to ensuring that people can exercise their reproductive rights.[70] The UN Special Rapporteur on the right to health has confirmed that criminalization of sexual and reproductive health services generates “a chilling effect on the open exchange of information,” and “[w]here narrow exceptions to the criminalization of abortion exist, such as to save the life of a woman, criminalization may effectively block access to information about legal abortion services.”[71] States have an obligation to provide access to comprehensive, accurate, and evidence-based information on abortion services, including on the legality of abortion and how to access safe abortion services and post-abortion care.[72] The right to information requires states to make this information accessible to all individuals, including adolescents and youth, without needing the consent of legal guardians.[73] States must ensure that health care providers give medically accurate and non-stigmatizing information on abortion, while also guaranteeing patient confidentiality.[74] And states also must ensure that information is accessible, and that people can seek, receive, and disseminate evidence-based, medically accurate, and unbiased information regarding abortion, as well as receive specific information on their individual health status.[75]
States have an obligation to provide access to comprehensive, accurate, and evidence-based information on abortion services, including on the legality of abortion and how to access safe abortion services and post-abortion care.
Consistent with these and other human rights protections (including the rights to equality and non-discrimination, privacy, and freedom from torture or cruel, inhuman, or degrading treatment), UN human rights treaty bodies have condemned the criminalization of abortion and expressed concern about the impact of severe legal restrictions and barriers on abortion access, as well as expressed concern about abortion stigma.[76] UN treaty bodies have urged states to provide financial support for those who cannot afford abortion services.[77] And the Human Rights Committee has recognized that national laws prohibiting abortion – thereby forcing people to choose between continuing a pregnancy and traveling to another country to access legal abortion services (for those able to travel) – can cause anguish and suffering, including financial, social, and health-related burdens and hardships.[78]
UN human rights law has increasingly recognized the state obligation to ensure that access to abortion includes full decriminalization.[79] UN treaty bodies and experts’ recommendations no longer only call for reform where states criminalize abortion without exceptions or in limited circumstances. Rather, such recommendations now explicitly urge full decriminalization, as well as positive measures to guarantee access to abortion, “at least” on specific grounds such as risk to life or health, for victims of rape and incest, and due to the existence of severe or fatal fetal impairment.[80]
U.S. regression on abortion rights, as exemplified by the abortion bans in Oklahoma, has been widely condemned as a violation of human rights. Responding to the U.S. Supreme Court’s decision in Dobbs v. Jackson Women’s Health Organization, then-UN High Commissioner for Human Rights Michelle Bachelet reiterated human rights protections for those seeking or providing abortions and the impact that the decision will have on the fundamental rights of millions within the United States, particularly people with low incomes and people belonging to racial and ethnic minorities.[81] UN independent human rights experts, including the UN Working Group on discrimination against women and girls, the UN Special Rapporteur on health, and the UN Special Rapporteur on violence against women, similarly denounced the decision in Dobbs.[82] At the conclusion of a human rights review of the United States in August 2022, the UN Committee on the Elimination of Racial Discrimination noted deep concerns with the Dobbs decision and recommended that the United States address the disparate impact that it will have on racial and ethnic minorities, Indigenous women, and those with low incomes.[83]
Medical Ethics Obligations of Health Care Professionals
In the United States, the professional membership organizations for professionals involved in reproductive and pregnancy-related health care are unambiguous in their opposition to laws that restrict their patients’ access to abortion services as part of their health care and that erect barriers to their members’ ability to practice evidence-based medicine. Professional organizations representing obstetrician-gynecologists, family physicians, and midwives, among the specialties involved in reproductive, prenatal, and peri- and postpartum care in the United States, are united in their reasons for opposing abortion laws like those in Oklahoma. Professional associations have denounced the threat of criminal liability under recent abortion bans for their potential chilling effect on the provision of evidence-based medical care in line with ethical obligations. For example, the American College of Obstetricians and Gynecologists (ACOG) has noted:
In states with laws criminalizing abortion provision, clinicians may be nervous to provide pregnant patients with needed diagnostic tests (i.e., radiology imaging) or interventions (i.e., anesthesia or surgical intervention for a ruptured appendix during pregnancy) due to fear of inadvertently causing a pregnancy loss. They may also be confused about the impact of abortion restrictions on miscarriage and pregnancy of unknown location management. In addition, they may be uncertain about what they should document in the medical record when caring for particular patients.[84]
ACOG has underscored the important role of hospitals in states with abortion bans in helping providers who seek to uphold medical standards of care and ethics:
It is important that clinicians feel supported by their hospitals to provide and connect pregnant patients with necessary care. This may involve setting up meetings between clinicians and the hospital’s legal counsel to review risks and discuss how the hospital will support and protect clinicians. It may also involve establishing hospital policies emphasizing clinicians’ responsibility to provide compassionate, evidence-based, and non-judgmental care to their patients in whatever way they can. Institutions can also bring in trainers to help clinicians understand best practices for preventing criminalization of pregnant patients who may present, for example, after self-managing an abortion.[85]
While these measures can help provide some support to clinicians navigating the legal and professional risks arising from these laws, ultimately, medical associations have affirmed the unworkability of these laws. ACOG has reaffirmed that “[d]octors and other health care professionals must be able to assess the unique patient and clinical situation in front of them and make reasonable, evidence-based decisions about when to intervene without fear of prosecution, loss of license, or fines.”[86]
“Doctors and other health care professionals must be able to assess the unique patient and clinical situation in front of them and make reasonable, evidence-based decisions about when to intervene without fear of prosecution, loss of license, or fines.”
American College of Obstetricians and Gynecologists
ACOG has unequivocally opposed “any effort that impedes access to abortion care and interferes in the relationship between a person and their health care professional. Because the patient-clinician relationship is a critical component of the provision of the highest quality health care, any efforts interfering in this relationship harm the people seeking essential health care and those providing it.”[87] It has specifically criticized state legislators “taking it upon themselves to define complex medical concepts without reference to medical evidence” and passing “vague, unscientific laws.” ACOG forcefully disagrees with the premise that “[e]lected politicians, who lack our members’ education, training, experience, expertise, and responsibility to patients, can or should be in the exam room weighing those factors or in a position of substituted judgment for our members and their patients.”[88]
ACOG’s position is echoed by the American Academy of Family Physicians (AAFP), the American College of Nurse-Midwives (ACNM), and the American Medical Association (AMA), among others.
In response to the Dobbs ruling, the AAFP, ACOG, the AMA, and 75 other health care organizations released a statement unequivocally opposing legislative interference in the patient-physician relationship. Like ACOG, the AAFP states that it “supports access to comprehensive pregnancy and reproductive services, including but not limited to abortion, pregnancy termination, contraception, and surgical and non-surgical management of ectopic pregnancy, and opposes nonevidence-based restrictions on medical care and the provision of such services.”[89] Similarly, the AAFP opposes legislation that infringes on the content or breadth of information exchanged within the patient-physician relationship and legislation that interferes with the provision of evidence-based medical care, either of which “can harm the health of the patient, the family, and the community.”[90]
The ACNM has joined with ACOG and AAFP in condemning laws restricting their patients’ access to abortion services as a necessary part of the “full-range of preventive, reproductive, and sexual health services.”[91] The ACNM affirms that “everyone has the right to decide what is best for their health, bodies, lives, and families. As such, we adamantly oppose all legal opinions and legislative policy that blatantly or surreptitiously seek to restrict or ban the provision of abortion care, as well as any efforts at any level to render it less accessible.”[92]
In response to new state laws such as those in Oklahoma, professional organizations are publishing new guidance for clinicians on how to navigate their dual loyalty constraints. The AMA, the largest membership organization of physicians across all specialties in the United States, revised its Principles of Medical Ethics in November 2022 to clarify that physicians are permitted to perform abortions as part of good medical practice. In their press release on the revised principles, the AMA noted that:
This is in alignment with the AMA’s opposition to government intrusion into the therapeutic alliance between patients and physicians, as such intrusion prevents physicians from exercising their professional judgment and undermines their obligation to protect the well-being of their patients.[93]
The AMA clarified its principles to recognize that where the “letter of the law would foreclose urgently needed care, physicians must have latitude to act in accord with their best professional judgment,” including explicitly in the context of abortion.[94]
The AMA has committed to providing support, including legal support, to physicians and medical students where needed and additional resources to help physicians navigate the ethical and legal aspects of the post-Dobbs era. AMA statements affirm the association’s commitment to oppose criminal charges against patients or physicians when pregnancy loss results from medically necessary treatment for cancer and other illnesses. The AMA also will advocate that physicians and patients should not be held civilly or criminally liable in cases when pregnancy loss results from medically necessary care. As Dr. Resneck succinctly described, “Under extraordinary circumstances, the ethical guidelines of the profession support physician conduct that sides with their patient’s safety and health, acknowledging that this may conflict with legal constraints that limit access to abortion or reproductive care.”[95]
Federal and State Legal Obligations
In support of these ethical guidelines, the federal government has clarified through Health and Human Services (HHS) guidance that the Emergency Medical Treatment and Active Labor Act (EMTALA) obligates physicians to provide stabilizing care, including abortion where medically appropriate, when a patient presenting at an emergency department is experiencing an emergency medical condition. While EMTALA indicates that abortion may be considered stabilizing care where needed to ensure that a patient will not have their health placed in serious jeopardy, have their bodily functions seriously impaired, or suffer serious dysfunction of any bodily organ or part, state laws are often more restrictive. State laws, as is the case in Oklahoma, may require that the individual’s life already be in danger prior to an abortion being permitted. HHS’s EMTALA guidance has been challenged by states with near abortion bans as being preempted by state law, with differing outcomes in different states.
The current legal framework in Oklahoma impedes hospitals and clinicians from fulfilling their ethical and professional responsibilities.
At the state level, Oklahoma law imposes stringent requirements for informed consent that are inconsistent with the hospitals’ inability to share information about what care patients may receive in certain circumstances.[96] Under Oklahoma Supreme Court precedent, a physician “should disclose all courses of treatment that are medically reasonable under the circumstances” and “is not permitted to withhold any facts which are necessary to form an intelligent consent by the patient to the proposed treatment.”[97] S.B. 1503, however, chills clinicians from sharing information with patients about abortion procedures by creating civil liabilities for anyone who “knowingly engages in conduct that aids or abets the performance or inducement of an abortion.”[98]
On September 21, 2022, the Oklahoma State Medical Association, ACOG, AMA, and the Society for Maternal-Fetal Medicine all signed an amicus curiae brief to the Oklahoma Supreme Court calling for an injunction of state abortion bans because they deprive individuals of their “inherent right to life [and] liberty,” particularly the right to bodily autonomy and integrity in making decisions about health care.[99] According to these organizations, “laws that criminalize and effectively ban abortion deprive pregnant patients of their rights to access a safe and essential component of reproductive health care without any medical or scientific justification.”[100]
Similarly, the American Bar Association “opposes governmental actions and policies that interfere with patients’ abilities to receive from their health care providers, including health care professionals and entities, in a timely manner: (a) all of the relevant and medically accurate information necessary for fully informed health care decision-making; and (b) information with respect to their access to medically appropriate care, as defined by the applicable medical standard of care, whether or not the provider chooses to offer such care.”[101]
In practice, the dual loyalties that clinicians face in states like Oklahoma are clear. Delaying access to abortion procedures until the patient is in a critical condition can result in the death of the patient or serious morbidities. On the other hand, providing a medically beneficial abortion before this point could result in criminal and financial penalties. The current legal framework in Oklahoma impedes hospitals and clinicians from fulfilling their ethical and professional responsibilities.
Conclusion and Recommendations
These findings affirm what has been recognized by the World Health Organization: that the criminalization and penalization of abortion care – even with an exception for medical necessity – is fundamentally inconsistent with evidence-based, ethical, and patient-centered health care, and with human rights.
Based on the findings of this report, not a single hospital in Oklahoma appeared to be able to articulate clear, consistent policies for emergency obstetric care that supported their clinicians’ ability to make decisions based solely on their clinical judgement or clearly explain how a prospective patient’s life would be prioritized or protected if faced with an obstetrical emergency. Oklahoma’s multiple, overlapping, and punitive abortion laws cause confusion regarding clinicians’ ability to provide health and life-saving care during obstetric emergencies without punishment.
These findings also underscore how health care providers in Oklahoma are placed in a situation of dual loyalty, forcing them to balance their obligation to provide ethical, high-quality medical care against the threat of legal and professional sanctions. Health professionals are effectively prevented from providing patient-centered care consistent with established medical and ethical standards of care, while pregnant people seeking obstetric care in the state are unable to obtain the information necessary to make informed decisions about their own health care. These risks are further compounded for populations already facing significant challenges and barriers in accessing essential medical care, including bias and discrimination.
Oklahoma’s abortion bans raise serious human rights concerns, including relating to violations of individuals’ rights to life, health, equality, information, freedom from torture and ill-treatment, and freedom to exercise reproductive autonomy. These findings affirm what has been recognized by the World Health Organization: that the criminalization and penalization of abortion care – even with an exception for medical necessity – is fundamentally inconsistent with evidence-based, ethical, and patient-centered health care, and with human rights.
Because the current legal status is untenable, Physicians for Human Rights, Oklahoma Call for Reproductive Justice, and the Center for Reproductive Rights make the following recommendations:
To the Oklahoma Legislature:
- Repeal Oklahoma’s abortion bans and decriminalize abortion. Remove all civil and legal penalties for abortion, including against health care providers.
- Ensure that health care services for pregnant people and all Oklahomans are accessible and of good quality. Policies should facilitate and expand, not limit, access to health care for people in Oklahoma. They should also address Oklahoma’s maternal mortality disparities and disparities in underlying social determinants of health that cause certain communities, including Black, Indigenous, and other Oklahomans of color, to experience adverse health outcomes.
To Oklahoma’s Hospitals and Health Care Professionals:
- Speak out against laws criminalizing abortion or otherwise restricting access to abortions, including during obstetric emergencies. Health care professionals and institutions should speak out about how abortion bans harm patients, undermine the ability of health care providers to fulfill their professional and ethical obligations, and are inconsistent with evidence-based, patient-centered, and ethical medical care.
- Build knowledge and awareness of professional recommendations and guidance for providing abortion services. Oklahoma hospitals and other health care providers must better ensure that staff and clinicians in clinical settings are acting in accordance with the recommendations that the American Medical Association (AMA), the American College of Obstetricians and Gynecologists (ACOG), and other medical professional organizations have made affirming ethical and professional obligations to provide abortion services to patients.
To State and National Medical Associations:
- Publicly condemn abortion bans and continue to speak out against the dual loyalty impacts of abortion bans, including citing evidence of how such laws undermine ethical obligations and professional duties of care. Associations such as the AMA and ACOG, including their state chapters, should advocate against this undue interference in the practice of medicine and engage at the state and national level to remove civil and legal penalties for abortion and maternal health care, and to secure rights.
To the Federal Government:
- Enact and implement national laws and policies that ensure rights and remove barriers to abortion care and maternal health care. Ensure that all people can access comprehensive reproductive health care with dignity, free from discrimination and criminalization, regardless of where they live.
To Professionals Who Provide Social, Legal, and Related Services to Pregnant People in Oklahoma and Nationally:
- Support pregnant people in navigating barriers to access the care they need. Social workers, mental health counselors, domestic violence assistance organizations, legal services providers, and other professionals should advocate for their clients to receive medically appropriate care, including abortions when necessary to preserve their health or life.
- Raise awareness of the discriminatory impacts and harms of laws criminalizing abortion. Professionals who provide support services to pregnant people are uniquely positioned to understand and speak out against the practical impact of abortion bans on their clients, including pregnant people for whom abortion may be necessary to preserve their health or life.
To Social Justice Advocates in Oklahoma and Nationally:
- Adopt an intersectional approach supporting solidarity in opposing abortion bans and supporting reproductive autonomy. Advocates for racial and economic justice, for bodily autonomy, for patients and providers, and for families and children should join reproductive health, rights, and justice advocates in opposing abortion bans and supporting pregnant people’s ability to access reproductive health care.
To Researchers and Research Institutes:
- Continue to systematically monitor and evaluate the impact of abortion bans on patients and providers. Build on existing research and share information to deepen awareness and understanding of the full scope of harms resulting from restrictive abortion laws and the criminalization of abortion services.
Acknowledgements
This report is a joint product of Physicians for Human Rights (PHR), the Oklahoma Call for Reproductive Justice (OCRJ), and the Center for Reproductive Rights (CRR).
The report was researched and written by PHR staff members Christian De Vos, JD, PhD, director of research and investigations; Michele Heisler, MD, MPA, medical director; William Jaffe, Aizik Wolf Fellow; and Payal Shah, JD, director of the Program on Sexual Violence in Conflict Zones; Tamya Cox-Touré, JD, OCRJ chair; and Priya Desai, MSW, OCRJ board member; and CRR staff members Nimra J. Chowdhry, JD, senior state legislative counsel; Risa Kaufman, JD, director, U.S. Human Rights; and Rabia Muqaddam, JD, senior staff attorney.
The report was reviewed by PHR staff members Erika Dailey, MA, director of advocacy and policy; Karen Naimer, MA, JD, LLM, director of programs; Ranit Mishori, MD, MHS, senior medical advisor; Michael Payne, deputy director, advocacy; Kevin Short, deputy director, media and communications; and Saman Zia-Zarifi, JD, LLM, executive director; and by Sandy Keenan, CRR’s senior director, marketing and communications. CRR staff members Tamar Eisen, program coordinator, Judicial Strategy; Lauren Elfant, JD, deputy director U.S. Program; Pilar Herrero, JD, senior human rights counsel; and Lourdes Rivera, JD, senior vice president U.S. Program Emerita also supported the project.
Calls to hospitals in Oklahoma were conducted by PHR graduate school interns Caytlin Schultz and Rachael Burton. Samantha Peck, PHR program and executive associate, also called hospitals and contributed to the writing of the report, as well as providing overall project support.
The report benefitted from external review by Angela Hawkins, MD, an obstetrics and gynecology specialist, and Susan M. Blaustein, MMA, DMA, PHR board member and founder/director of WomenStrong.
The report was reviewed, edited, and prepared for publication by Claudia Rader, MS, PHR’s senior publications consultant.
PHR, OCRJ, and CRR are grateful for the efforts of staff at the Oklahoma hospitals that were contacted, who took time to answer callers’ questions.
Endnotes
[1] Press release, Department of Justice, Garland Statement on Supreme Court Ruling in Dobbs v. Jackson Women’s Health Organization (Jun. 24, 2022), https://www.justice.gov/opa/pr/attorney-general-merrick-b-garland-statement-supreme-court-ruling-dobbs-v-jackson-women-s.
[2] “Heartbeat” is an inaccurate term referring to the rudimentary electrical activity that occurs around five or six weeks in an embryo or fetus. The embryo or fetus at that stage has not developed a “heart.” See also 63 Okla. Stat. §§ 1-745.34-45; 21 Okla. Stat. § 861; 63 Okla. Stat. §§ 1-731.4.
[3] As used in this report, the term “abortion bans” refer to prohibitions of abortion after conception. Restrictions on abortion after a certain number of weeks (“gestational limits”) are not included in this term. There are additional states beyond the 13 identified where laws banning abortions have been written but are not in effect, due to court injunctions or opposition by state governors and attorneys general. See also, After Roe Fell: Abortion Laws by State, Center for Reproductive Rights (CRR), https://reproductiverights.org/maps/abortion-laws-by-state/.
[4] Ark. Code Ann. § 5-61-301 to –304; See, e.g., After Roe Fell: Arkansas, CRR, https://reproductiverights.org/maps/state/arkansas/.
[5] Miss. Code Ann. § 41-41-45; See, e.g., After Roe Fell: Mississippi, CRR, https://reproductiverights.org/maps/state/mississippi/.
[6] S.D. Codified Laws § 22-17-5.1; See, e.g., After Roe Fell: South Dakota, CRR, https://reproductiverights.org/maps/state/south-dakota/.
[7] Alyssa Llamas et al., Jacobs Inst. of Women’s Health, Geo. Wash. Univ. & the Clara Schiffer Project on Women’s Health, Public Health Impacts of State-level Abortion Restrictions Overview of Research & Policy in the United States 1, (Apr. 2018), https://publichealth.gwu.edu/sites/default/files/downloads/projects/JIWH/Impacts_of_State_Abortion_Restrictions.pdf; Erin Durkin, ‘Women Will die’: How New Abortion Bans Will Harm the Most Vulnerable, The Guardian (May 19, 2019), https://www.theguardian.com/us-news/2019/may/19/abortion-ban-alabama-women-of-color-poor; Liza Fuentes, Latina Immigrant Women’s Access to Abortion: Insights from Interviews with Latina Grasstops Leaders, Nat’l Latina Inst. for Reprod. Health 1-4 (Sep. 2010), https://nciwr.files.wordpress.com/2011/01/nlirh-reserach-brief-sept2010-final1.pdf; National Council on Disability, The Current State of Health Care for People with Disabilities 51–52, 54–56, (2009), https://ncd.gov/publications/2009/Sept302009#Health%20Status; Megan K. Donovan, In Real Life: Federal Restrictions on Abortion Coverage and the Women They Impact, Guttmacher Inst. (Jan. 5, 2017), https://www.guttmacher.org/gpr/2017/01/real-life-federal-restrictions-abortion-coverage-and-women-they-impact.
[8] These states are Arkansas, Oklahoma, South Dakota, and Texas, see State Bans on Abortion Throughout Pregnancy, Guttmacher Inst. (Feb. 1, 2023), https://www.guttmacher.org/state-policy/explore/state-policies-later-abortions.
[9] Alabama, Kentucky, Missouri, and Tennessee have exceptions for only life and health (“severe permanent damage to major organs or bodily functions”). Louisiana and West Virginia currently have exemptions for a list of fetal anomalies in addition to life and health. Idaho and West Virginia have rape exceptions in addition to life and health, Mississippi has a rape exception in addition to life, and Idaho and West Virginia also have incest exceptions in addition to life and health, see ibid.
[10] In the face of concerns about the vagueness of exceptions, several lawmakers have attempted to create lists of specific conditions or criteria under which abortion is legally permitted. However, this approach fails for several reasons. First, pregnancy is a complex condition, and it is impossible to contemplate every circumstance that may come up where a termination may be clinically indicated. See, e.g., Understanding and Navigating Medical Emergency Exceptions in Abortion Bans and Restrictions, Am. Coll. of Obstetricians and Gynecologists (ACOG) (Aug. 15, 2022), https://www.acog.org/news/news-articles/2022/08/understanding-medical-emergency-exceptions-in-abortion-bans-restrictions (outlining why lists of conditions that qualify as “medical emergencies” are impossible to create and are unworkable). Second, even where there is a list of criteria or conditions, there may still be confusion around the certainty or severity of the diagnosis. See, e.g. World Health Org., Abortion Care Guideline, 21-30 (2022), https://www.who.int/publications/i/item/9789240039483. Third, it is clear from international human rights jurisprudence that even where countries have broad exceptions, the continued criminalization of abortion continues to hinder abortion access by creating stigma and fear amongst health care providers. See, e.g., Comm. on the Elimination of Discrimination against Women (CEDAW), Inquiry Concerning the United Kingdom of Great Britain and Northern Ireland under article 8 of the Optional Protocol to the Convention on the Elimination of All Forms of Discrimination against Women, ¶¶17-20, U.N. Doc. CEDAW/C/OP.8/GBR/1 (Mar. 6, 2018); CEDAW, Concluding Observations on the Sixth Periodic Report of Nepal, ¶¶ 38-39, UN Doc. CEDAW/C/NPL/CO/6 (Nov. 14, 2018).
[11] See Physicians for Human Rts. & the Sch. of Pub. Health and Primary Health Care Univ. of Cape Town, Dual Loyalty & Human Rights In Health Professional Practice: Proposed Guidelines & Institutional Mechanisms, 11-13 (2002), https://phr.org/wp-content/uploads/2003/03/dualloyalties-2002-report.pdf.
[12] Press Release, AMA announces new adopted policies related to reproductive health care, AMA, (Nov. 16, 2022), https://www.ama-assn.org/press-center/press-releases/ama-announces-new-adopted-policies-related-reproductive-health-care.
[13] Anita Wadhwani, “In open Letter, 700 Tennessee healthcare providers call on Legislature to ‘reconsider’ abortion ban,” Tennessee Lookout(Oct. 10, 2022), https://tennesseelookout.com/briefs/in-open-letter-700-tennessee-healthcare-providers-call-on-legislature-to-reconsider-abortion-ban/.
[14] Piper Hutchinson, “Doctors spell out their opposition to Louisiana’s abortion law,” Louisiana Illuminator (Jul. 6, 2022), https://lailluminator.com/2022/07/06/doctors-spell-out-their-opposition-to-louisianas-abortion-law/.
[15] See Prelabor Rupture of Membranes, ACOG (Mar. 2020), https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2020/03/prelabor-rupture-of-membranes; See also, What are some common complications of pregnancy?, NICHD Eunice Kennedy Shriver Nat’l Inst. of Child Health and Hum. Dev., https://www.nichd.nih.gov/health/topics/pregnancy/conditioninfo/complications.
[16] Carla Dugas & Valori H. Slane, Miscarriage, (Jun. 27, 2022), https://www.ncbi.nlm.nih.gov/books/NBK532992/.
[17] Rosemary Westwood, “Bleeding and in pain, she couldn’t get 2 Louisiana ERs to answer: Is it a miscarriage?,” NPR (Dec. 29, 2022), https://www.npr.org/sections/health-shots/2022/12/29/1143823727/bleeding-and-in-pain-she-couldnt-get-2-louisiana-ers-to-answer-is-it-a-miscarria.
[18] As noted above, “heartbeat” is an inaccurate term referring to the rudimentary electrical activity that occurs around five or six weeks in an embryo or fetus. Six-week gestational limits use the term “fetal heartbeat,” although the embryo or fetus at that stage has not developed a “heart.”
[19] Mikhaila Richards, The Public, Including Women of Childbearing Age, Are Largely Confused About the Legality of Medication Abortion and Emergency Contraceptives in Their States, Kaiser Family Foundation (Feb. 1, 2023), https://www.kff.org/womens-health-policy/press-release/the-public-including-women-of-childbearing-age-are-largely-confused-about-the-legality-of-medication-abortion-and-emergency-contraceptives-in-their-states/.
[20] Nicole Einbinder and Caroline Haskins, “Oklahoma lawmakers passed 5 contradictory abortion bans. No one knows which laws will be enforced,” Business Insider (Jun. 24, 2022), https://www.businessinsider.com/oklahoma-abortion-ban-sponsors-dont-know-what-law-might-be-post-roe-2022-5?op=1.
[21] See Memorandum from Okla. Att’y Gen. to All Okla. Law Enf’t Agencies, Guidance for Okla. law enforcement following Dobbs v. Jackson Women’s Health Org, (Aug. 31, 2022) (“Guidance”).
[22] See ibid.
[23]63 Okla. Stat. §§ 1-745.34(A).
[24] 63 Okla. Stat. §§ 1-745.39(A).
[25] See 63 Okla. Stat. §§ 1-745.51-60; 63 Okla. Stat. §§ 1-745.51-52.
[26] Oklahoma S.B. 1555.
[27] 21 Okla. Stat. § 861.
[28] 63 Okla. Stat. § 1-731.4.
[30] See, e.g., 59 Okla. Stat. §§ 509, 509.1 (providing for professional sanctions against physicians).
[31] For clinicians, see e.g., 59 Okla. Stat. §§ 509, 509.1.
[32] 63 Okla. Stat. § 1-731.4; 63 Okla. Stat. §§ 1-745.51-52.
[33] 63 Okla. Stat. § 1-745.31.
[34] 21 Okla. Stat. § 861.
[35] 21 Okla. Stat § 691.
[36] 63 Okla. Stat. § 1-745.52
[37] See Gender Equity Pol. Inst., The State of Reproductive Health in the United States: The End of Roe and the Perilous Road Ahead for Women in the Dobbs Era (Jan. 19, 2023) at 6, https://thegepi.org/wp-content/uploads/2023/01/GEPI-State-Repro-Health-Report.pdf; Donna L. Hoyert, Maternal Mortality Rates in the United States, 2021, CDC (Mar. 2023), https://www.cdc.gov/nchs/data/hestat/maternal-mortality/2021/maternal-mortality-rates-2021.htm.
[38] Katherine Ellison and Nina Martin, “Severe Complications for Women During Childbirth Are Skyrocketing — and Could Often Be Prevented,” ProPublica (Dec. 22, 2017),https://www.propublica.org/article/severe-complications-for-women-during-childbirth-are-skyrocketing-and-could-often-be-prevented.
[39] See, e.g.,Jamila K. Taylor, Structural Racism and Maternal Health Among Black Women,48 J. L., Med. & Ethics 506 (2020), https://doi.org/10.1177/1073110520958875; Saraswathi Vedam et al., The Giving Voice to Mothers Study: Inequity and Mistreatment During Pregnancy and Childbirth in the United States,16 Reprod. Health, 77 (2019), https://doi.org/10.1186/s12978-019-0729-2; Judith A. Lothian, The Continued Mistreatment of Women During Pregnancy and Childbirth, 28 J. Perinatal Educ., 183 (2019), DOI: 10.1891/1058-1243.28.4.183.
[40] See Gender Equity Policy Institute, supra note 37 at 3.
[41] Ibid. at 8-10.
[42] Ibid.
[43] Okla. State Dep’t of Health, Okla. Maternal Mortality Rev. Comm., Oklahoma Maternal Health, Morbidity and Mortality: Annual Report 2021, at 5, 26 (2021),
https://oklahoma.gov/content/dam/ok/en/health/health2/aem-documents/family-health/maternal-and-child-health/maternal-mortality/maternal-morbidity-mortality-annual-report-2021.pdf.
[44] Okla. State Dep’t of Health, Okla. Maternal Mortality Rev. Comm., Maternal Mortality in Oklahoma 2004-2018, at 4 (2020), https://oklahoma.gov/content/dam/ok/en/health/health2/aem-documents/family-health/maternal-and-child-health/maternal-mortality/annual-mmrc-report.pdf.
[45] Ibid.
[46] Notably, the study does not address the larger population of people whose rights to abortion have also been affected by Oklahoma’s legal regime, such as those seeking non-emergency abortions due to other medical conditions or fetal anomalies.
[47] This research methodology is also referred to as a “secret shopper” methodology and has been used as well in multiple consumer and employment studies to document discrimination based on gender, race, and ethnicity (e.g., in examining housing practices based on the race of a prospective renter or buyer).
[48] See, e.g., Pooja A. Lagisetty et al., Access to Primary Care Clinics for Patients With Chronic Pain Receiving Opioids, 2 Jama Network Open (Jul. 3, 2019), doi: 10.1001/jamanetworkopen; Brent R. Asplin et al, Insurance status and access to urgent ambulatory care follow-up appointments, 29 J. of the Am. Med. Ass’n 1248-1254 (Sep. 14, 2005), doi:10.1001/jama.294.10.1248; Karin V. Rhodes & Franklin G. Miller, Simulated patient studies: an ethical analysis, 90 The Milbank Q. 706-724 (Dec. 2012), doi: 10.1111/j.1468-0009.2012.00680.x.
[49] PHR’s Ethics Review Board provided guidance and approved this study based on regulations outlined in Title 45 CFR Part 46, which are used by academic Institutional Review Boards in the United States. All of PHR’s research and investigations involving human subjects are conducted in accordance with the Declaration of Helsinki 2000, a statement of ethical principles for medical research involving human subjects, including research on identifiable human material and data.
[50] See Oklahoma Hospital Directory, Oklahoma Hospital Ass’n, https://www.okoha.com/OHA/Hospital_Directories/OHA/Directory/Hospital_List_Public.aspx?hkey=d87455ef-ec45-49ac-8fd6-fff05ad0116c; Hospitals and Medical Facilities in Oklahoma, OfficialUSA.com https://www.officialusa.com/stateguides/health/hospitals/oklahoma.html.
[51] The Hyde Amendment is a legislative provision, included in Congressional spending bills since 1976, that prohibits federal funds from covering abortion services for people enrolled in Medicaid, Medicare, and CHIP. As a result, Medicaid enrollees are not covered for abortion services in the 34 states (and Washington, D.C.) that do not allocate state funds to extend coverage. Currently, 7.8 million women aged 15-49 with Medicaid coverage lack abortion coverage. Half of those affected are women of color. See The Hyde Amendment: A Discriminatory Ban on Insurance Coverage of Abortion, Guttmacher Inst.(May 2021), https://www.guttmacher.org/fact-sheet/hyde-amendment.
[52] Using the definitions given by the U.S. Census Bureau, hospitals are classified as “heavily urbanized” if the town population exceeds 50,000 people. The “non-urban” category combines the “urban cluster” (2,500 – 50,000 people) and “rural” (less than 2,500 people) definitions to create a large enough sample size. See 2010 Census Urban and Rural Classification and Urban Area Criteria, United States Census Bureau, https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural/2010-urban-rural.html.
[53] Hospitals with fewer than 100 beds in their entire facilities are classified as “small,” those with between 100 and 500 beds are coded as “medium,” and those with more than 500 beds are considered “large.”
[54] Facilities were divided into the following regions, based on their proximity to major urban centers: “Northern” hospitals were those located in the Tulsa metropolitan area; “Central” hospitals were those located in the Oklahoma City metropolitan area; “Eastern” hospitals were those south of Tulsa and east of Oklahoma City; and “Southern” and “Western” hospitals were located south and west, respectively, of the Oklahoma City metropolitan area. All hospital names, locations, and other potentially identifying information have been de-identified in this report.
[55] For the purpose of this study, the team opted to portray the pregnant patients as cisgender women.
[56] Oklahoma Uninsured Fast Facts CY 2021, Oklahoma Health Authority (Nov. 28, 2022), https://oklahoma.gov/content/dam/ok/en/okhca/docs/research/data-and-reports/fast-facts/2023/january/Uninsured%20Fast%20Fact%20CY2021_nov2022.pdf.
[57] Procedures to remove ectopic pregnancies should not be considered “abortions” because the implanted egg is never viable and always poses a life-threatening danger that must be terminated as soon as possible. Failing to make this distinction suggests that ectopic pregnancies fall under the abortion legal framework, which would require doctors to wait until the patient enters a life-threatening state, at which point it could be too late to act. This confusion could be exacerbated by the fact that one of the abortion bans explicitly includes a separate exception for ectopic pregnancies, even though management of an ectopic pregnancy is not medically considered an abortion, while the other bans are silent on cases of ectopic pregnancy. See Tubal Ectopic Pregnancy, ACOG, (Mar. 18, 2018), https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2018/03/tubal-ectopic-pregnancy.
[58] See, e.g., Understanding and Navigating Medical Emergency Exceptions, supra note 10; Abortion Policy: Statement of Policy, ACOG, (May 2022), https://www.acog.org/clinical-information/policy-and-position-statements/statements-of-policy/2022/abortion-policy; Questions to Help Hospital Systems Prepare for the Widespread and Devastating Impacts of a Post-Roe Legal Landscape, ACOG, (Jun. 24, 2022), https://www.acog.org/news/news-articles/2022/06/questions-to-help-hospital-systems-prepare-for-the-widespread-and-devastating-impacts-of-a-post-roe-legal-landscape.
[59] The United States has ratified three core human rights treaties with important protections for reproductive autonomy: the International Covenant on Civil and Political Rights (ICCPR), opened for signature Dec. 19, 1966, 99 U.N.T.S. 171; the Convention Against Torture and Other Cruel, Inhuman, or Degrading Treatment or Punishment (CAT), opened for signature Dec. 10, 1984, 1465 U.N.T.S. 85; and the Convention on the Elimination of All Forms of Racial Discrimination (CERD), opened for signature Dec. 21, 1965, 660 U.N.T.S. 195. The United States has signed but not yet ratified several other human rights treaties that likewise contain critical protections for reproductive autonomy, including the International Covenant on Economic, Social and Cultural Rights (ICESCR), opened for signature Dec. 16, 1966, 993 U.N.T.S. 3; the Convention on the Elimination of All Forms of Discrimination Against Women (CEDAW), opened for signature Dec. 18, 1979, 1249 U.N.T.S. 13; and the Convention on the Rights of Persons with Disabilities (CRPD), adopted on Dec. 13, 2006, 2515 U.N.T.S. 3.
[60] See CRR, Breaking Ground: Treaty Monitoring Bodies on Reproductive Rights 2016, 22 (2016), https://reproductiverights.org/wp-content/uploads/2020/12/GLP_TMB_Booklet_2016_Web.pdf; CRR, Breaking Ground: Treaty Monitoring Bodies on Reproductive Rights 2020, 12 (2019), https://reproductiverights.org/sites/default/files/documents/Breaking-Ground-2020.pdf. See also World Health Organization, Abortion Care Guideline Web Annex A. Key International Human Rights Standards on Abortion (2022), https://apps.who.int/iris/bitstream/handle/10665/349317/9789240039506-eng.pdf.
[61] World Health Organization (WHO), Abortion Care Guideline, 13-14 (2022), https://www.who.int/publications/i/item/9789240039483; CRR, WHO’s New Abortion Guideline: Highlights of Its Law and Policy Recommendations (Mar. 2022), https://reproductiverights.org/wp-content/uploads/2022/03/CRR-Fact-sheet-on-WHO-Guidelines.pdf.
[62] See Comm. on Econ., Soc. and Cultural. Rts., General Comment No. 22: On the right to sexual and reproductive health (Art. 12 of the International Covenant on Economic, Social and Cultural Rights) U.N. Doc. E/C, 12/GC/22 (May 2, 2016) [hereinafter ICESCR, General Comment 22].
[63] ICESCR, General Comment 22 at ¶¶ 12-21.
[64] In the international context, such as in the United Nations, the term “states” refers to national governments (i.e. “state parties”). However, elsewhere in the report, the term “states” is used to refer to the sub-national governments within the United States. See UN Hum. Rts. Comm., General Comment No. 36: On Article 6 of the International Covenant on Civil and Political Rights, on the right to life, U.N. Doc. CCPR/C/GC/36, at ¶ 8 (Sep. 3, 2019), https://www.ohchr.org/sites/default/files/Documents/HRBodies/CCPR/CCPR_C_GC_36.pdf. [hereinafter referred to as HRC, General Comment No. 36]
[65] See generally World Health Organization, Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health (2008), https://apps.who.int/iris/bitstream/handle/10665/43943/9789241563703_eng.pdf;jsessionid=5C0ACAD105BC140CFA4FFFA3CA8F9A31?sequence=1.
[66] Abortion, WHO, (Nov. 15, 2021), https://www.who.int/news-room/fact-sheets/detail/abortion.
[67] See, e.g., HRC, General Comment No. 36; ICESCR General Comment 22; OHCHR, CRC General Comment No. 4: Adolescent health and development, UN Doc. CRC/GC/2003/4 (Jul. 1, 2003); CEDAW, General Recommendation No. 34, on the Rights of rural women, UN Doc. CEDAW/C/GC/34 (2016). See also Special Rapporteur on extrajudicial, summary or arbitrary executions, Report of the Special Rapporteur on extrajudicial, summary or arbitrary executions on a gender-sensitive approach to arbitrary killings, UN Doc. A/HRC/35/23 (2017) (“States should remove undue restrictions on access to safe and legal abortions that may threaten women and girls’ right to life and to health”).
[68] See HRC, General Comment No. 36, at ¶ 8.
[69] See Brief for UN Mandate Holders as Amici Curiae Supporting Respondents, Dobbs v. Jackson Women’s Health Org., No. 19-1392 (U.S. Sep. 20, 2021), at 31-32.
[70] See, e.g., ICESCR, General Comment 22, at ¶ 18; Committee on the Rights of Persons with Disabilities, General Comment No. 3: Women and Girls with disabilities, ¶ 40; Convention on the Elimination of All Forms of Discrimination Against Women (CEDAW), Art. 10, ¶ H; CEDAW Committee, General Recommendation No. 24, ¶ 28. See also ICCPR, art. 19, ¶ 2.
[71] Interim report of the Special Rapporteur on the right of everyone to the highest attainable standard of physical and mental health, UN Doc. A/66/254 (2011), https://undocs.org/en/A/66/254.
[72] ICESCR, General Comment 22, at ¶¶18-21, 40-41, 43-44.
[73] Ibid, at ¶¶ 18-21, 44.
[74] ICESCR General Comment 22, at ¶ 19; HRC, General Comment No. 36, ¶ 8; Committee on the Rights of the Child, Concluding Observations: Slovakia, ¶ 41(e), U.N. Doc. CRC/C/SVK/CO/3-5 (2016).
[75] See ICESCR, General Comment 22, at ¶ 18-21.
[76] See CRR, Breaking Ground: 2020, supra note 60, at 12-15.
[77] Ibid. at 14.
[78] See Hum. Rts. Comm., Siobhán Whelan v Ireland: Views Adopted by the Committee Under Article 5 (4) of the Optional Protocol, Concerning Communication No. 2425/2014, ¶¶ 7.5–7.7, 7.9, 7.11–7.12, U.N. Doc. CCPR/C/119/D/2425/2014 (2017); Hum. Rts. Comm., Amanda Jane Mellet v Ireland: Views Adopted by the Committee under Article 5 (4) of the Optional Protocol, Concerning Communication No. 2324/2013, ¶¶ 7.4–7.6, 7.8, 7.10–7.11, U.N. Doc. CCPR/C/116/D/2324/2013 (2016).
[79] See Hum. Rts. Comm., Mellet v Ireland, Comm. No. 2324/2013, UN Doc. CCPR/C/116/D/2324/2013 (2016). See also CRR, Breaking ground: 2020, at 13, 25. See also Johanna B. Fine et al., The role of international human rights norms in the liberalization of abortion laws globally, Health and Human Rights Journal (2017), www.hhrjournal.org/2017/06/the-role-of-international-human-rights-norms-in-the-liberalization-of-abortion-laws-globally/.
[80] Kamala Chandrakirana, Chair-Rapporteur of the Working Grp. on the Issue of Discrimination against Women in Law and in Practice et al., International Safe Abortion Day – Thursday 28 September 2017, UN Office of the High Comm. For Hum Rts. (Sep. 27, 2017), www.ohchr.org/EN/NewsEvents/Pages/DisplayNews.aspx?NewsID=22167&LangID=E; CRPD and CEDAW, Guaranteeing sexual and reproductive health and rights for all women, in particular women with disabilities (Aug. 29, 2018), https://www.ohchr.org/en/treaty-bodies/crpd/statements-declarations-and-observations; Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, Interim rep. of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, transmitted by Note of the Secretary-General, ¶ 65(h), (i), UN Doc. A/66/254 (2011); CEDAW, Concluding Observations on the combined eighth and ninth periodic reports of Haiti, UN Doc. CEDAW/C/HTI/CO/8-9 (2016); CEDAW, Concluding observations on the combined seventh and eighth periodic reports of Honduras, UN Doc. CEDAW/C/HND/CO/7-8 (2016). See also CRC, Concluding Observations on the combined fourth and fifth periodic reports of Mexico, UN Doc. CRC/C/MEX/CO/4-5 (2015).
[81] Michelle Bachelet, Comment by UN High Commissioner for Human Rights Michelle Bachelet on US Supreme Court Ruling on Dobbs v Jackson Women’s Health Organization (Jun. 24, 2022), https://www.ohchr.org/en/statements/2022/06/bachelet-us-ruling-dobbs-v-jackson-womens-health-organization.
[82] Melissa Upreti et al., Joint Web Statement by UN Human Rights Experts on Supreme Court Decision to Strike Down Roe v. Wade, Working Grp. on Discrimination Against Women and Girls, Special Rapporteur on the Right of Everyone to the Enjoyment of the Highest Attainable Standard of Physical and Mental Health & Special Rapporteur on Violence Against Women, Its Causes and Consequences, (Jun. 24, 2022), https://www.ohchr.org/en/statements/2022/06/joint-web-statement-un-human-rights-experts-supreme-court-decision-strike-down.
[83] CERD., Concluding observations on the combined tenth to twelfth reports of the United States of America, ¶¶ 35-36, CERD/C/USA/CO/10-12 (Aug. 30, 2022).
[84] Questions to Help Hospital Systems, supra note 58.
[85] Ibid.
[86] Understanding and Navigating Medical Emergency Exceptions, supra note 10.
[87] Abortion Policy: Statement of Policy, supra note 58.
[88] Understanding ACOG’s Policy on Abortion, ACOG, (May 23, 2022), https://www.acog.org/news/news-articles/2022/05/understanding-acog-policy-on-abortion.
[89] More Than 75 Health Care Organizations Release Joint Statement in Opposition to Legislative Interference, ACOG, (Jul. 7, 2022), https://www.acog.org/news/news-releases/2022/07/more-than-75-health-care-organizations-release-joint-statement-in-opposition-to-legislative-interference.
[90] In a July 13, 2022 letter to the Senate Judiciary Committee, Ada D. Stewart, Board Chair, American Academy of Family Physicians, expressed concern that, “Cases…. in which patients experience delay or denial as they seek critical and in some cases lifesaving care, will multiply. The result will be worse health outcomes and greater health disparities nationwide.” See Ada D. Stewart, American Academy of Family Physicians, Testimony to the Hearing on Reproductive Care in a Post-Roe America: Barriers, Challenges, and Threats to Women’s Health, S. Comm. on Health Educ. Lab. & Pensions, 117th Cong. 4 (Jul. 13, 2022), https://www.aafp.org/dam/AAFP/documents/advocacy/prevention/women/TS-SenateHELP-PostRoe-071322.pdf.
[91] Statement: ACNM Condemns SCOTUS Decision, Dobbs v. Jackson Women’s Health Organization, Am. Coll. of Nurse-Midwives (Jun. 24, 2022),https://www.midwife.org/statement-acnm-condemns-scotus-decision-dobbs-v.-jackson-women-s-health-organization.
[92] Ibid.
[93] Press Release, AMA announces new adopted policies, supra note 12.
[94] Kevin B. O’Reilly, AMA holds fast to principle: Reproductive care is health care, AMA, (Nov. 16, 2022), https://www.ama-assn.org/delivering-care/public-health/ama-holds-fast-principle-reproductive-care-health-care.
[95] Press Release, AMA announces new adopted policies, supra note 12.
[96] Allen v. Harrison, 374 P.3d 812, ¶ 10 (2016).
[97] Scott v. Bradford, 606 P.2d 554, ¶ 18 (1979) (internal quotation omitted).
[98] 63 Okla. Stat. §§ 1-745.39(A).
[99] Brief for Am. Coll. of Obstetricians and Gynecologists, Am. Med. Ass’n, Okla. State Med. Ass’n, Soc’y for Maternal-Fetal Med. as Amici Curiae Supporting Respondents, Oklahoma Call for Reproductive Justice et al. v. John O’Conner et al., No. PR-120543 (filed Sep. 21, 2022), https://www.ocpathink.org/uploads/assets/pdfs/1053478446-20220921-144041.pdf; Oklahoma Const. art. II, § 2.
[100] Ibid.
[101] Stephen F. Hanlon, Res.Am. Bar Ass’n (Feb. 14, 2005), https://www.americanbar.org/content/dam/aba/directories/policy/midyear-2005/2005_my_104.pdf.


