Physicians for Human Rights (PHR) and the Cardozo Law Institute in Holocaust and Human Rights (CLIHHR) are pleased to provide this submission in response to the International Criminal Court (ICC) Office of the Prosecutor’s (OTP) Call for Updates of the OTP 2014 Policy Paper on Sexual and Gender-Based Crimes (2014 Policy Paper). The 2014 Policy Paper was a groundbreaking step forward in articulating the commitment of the OTP to prioritize redress for sexual and gender-based crimes (SGBC) and address barriers to achievement of this vision. This, along with the 2022 Policy on the Crime of Gender Persecution, establishes the commitment of the OTP to adopt a gender-competent perspective and to prioritize accountability for SGBC. As an organization committed to addressing SGBC, PHR and CLIHHR offer this submission to suggest how the 2014 Policy Paper can be updated and further developed to articulate key principles in addressing SGBC occurring during and outside of conflict.
What Constitutes a High-Quality, Comprehensive Medico-Legal Affidavit in the United States Immigration Context?
This fact sheet summarizes the findings of the first published multi-sectoral consensus-building exercise on medico-legal affidavits in the U.S. immigration context. Medico-legal affidavits are underpinned by an expert medical evaluation which can objectively contextualize trauma and corroborate accounts of abuse; they are a critical component in immigration proceedings where somebody is seeking protection on the basis of said trauma or abuse. However, the lack of existing validated guidelines has led to inconsistencies in clinical evaluations’ format, structure, and content, causing confusion for practitioners and adjudicators alike. Drawing on expertise from adjudicators, attorneys, and clinicians, this Physicians for Human Right (PHR) research therefore aimed to pinpoint what experts viewed as the most crucial aspects of medico-legal asylum evaluations and their accompanying affidavits. By using a modified Delphi approach to collect and synthesize expert opinions, a consensus was reached on the defining features of a high-quality, comprehensive evaluation. The study identified seven key areas that were most agreed upon by participants, which serve as a foundation for future efforts to standardize and enhance the overall quality and consistency of medico-legal reports.
Voicing Our Plight
Using Photovoice to Assess Perceptions of Mental Health Services for Survivors of Sexual Violence in Kenya
Executive Summary
Background
Sexual and gender-based violence (SGBV) is a global health crisis. More than 730 million women worldwide have experienced physical or sexual violence at least once in their lifetime.[1] In Kenya, the Demographic and Health Survey of 2022 showed that 34 percent of women and girls[2] surveyed reported having experienced physical violence at least once in their lifetime and 13 percent reported having experienced sexual violence, with many of these cases going unreported to authorities.[3] SGBV has profound impacts on a survivor’s physical and mental health.[4] Access to mental health care is a major challenge for survivors of sexual violence.[5]
In Kenya, 34 percent of women and girls aged 15-49 years surveyed have experienced physical violence at least once in their lifetime and 13 percent have experienced sexual violence, with many of these cases going unreported. SGBV has profound impacts on survivors’ physical and mental health, and access to mental health care is a major challenge for survivors of sexual violence.

Physicians for Human Rights’ Program on Sexual Violence in Conflict Zones began working in Kenya in 2011 to confront impunity for sexual violence committed during the unrest that followed the 2007 national elections.
From 2020 to 2022, PHR worked with partners, including the Survivors of Sexual Violence Network in Kenya (SSVKenya) convened by the Wangu Kanja Foundation, to address challenges faced by survivors. These included medical-legal documentation of the mental health impacts of sexual violence and access to quality mental health services in Kenya. The project, supported by the Comic Relief & UK Aid Mental Health Programme, aimed to enhance the capacities of health professionals and institutions in Kenya to provide post-rape mental health care and to forensically document the mental health impacts of sexual violence, as well as to strengthen the legal and policy framework on mental health care in Kenya.
This assessment arose out of PHR’s interest in understanding the impact of these interventions and related advocacy from the perspective of survivors of sexual violence, themselves. To ensure the voices of survivors remained at the heart of the assessment, PHR partnered with SSVKenya, an advocacy coalition comprised of survivors of sexual violence in Kenya.


Methodology
To conduct the assessment, PHR and SSVKenya jointly identified 10 survivors of sexual violence from across Nairobi who lived in areas that benefitted from the intervention, were active in SSVKenya, and were engaged in their communities as activists, human rights defenders, and volunteers helping other survivors access health services.
The assessment team selected Photovoice – a participatory action research (PAR) methodology through which community members document their experiences using photography – as well as voice recordings for this assessment.
The use of this methodology reflected a deliberate choice to empower survivors and mitigate the risk of re-traumatization that is inherent in traditional, interview-driven methodologies. The assessment team included self-selected survivors who were motivated to document issues important to them and their community and three PHR staff members. Using this methodology, survivors were equal partners in the assessment.[9],[10]

The assessment team selected Photovoice – a participatory action research (PAR) methodology through which community members document their experiences using photography. Using this methodology, survivors were equal partners in the assessment.
Findings
The assessment team took a total of 223 photos during a one-week period in October and November 2022 representing their experiences accessing mental health services in Nairobi. These photos were accompanied by a total of 99 WhatsApp voice notes.
Analysis of these materials, conducted by the assessment team and the survivor-collaborators, showed that survivors perceived gaps in the availability, accessibility, acceptability, and quality (AAAQ) of mental health services. As the AAAQ are the essential elements to realizing the right to health, they provide a powerful framework to understand sexual violence-related mental health services from a rights-based perspective.[12]
Availability
Survivors said mental health services for survivors of sexual violence are often unavailable in their communities, due to closed facilities, missing staff, or infrastructure challenges. They said there is minimal prioritization of mental health care services in general, and specifically of services targeting survivors of SGBV and other vulnerable groups.
Accessibility
Survivors identified difficulties accessing mental health services across Nairobi, with transportation a major challenge. They also experienced challenges accessing private facilities, primarily due to the high cost of mental health services and medication.
Acceptability
Survivors felt that many services being offered were not acceptable for their particular needs, including lack of private spaces for counselling sessions. They feared breaches of confidentiality and others learning about their history of sexual violence. They also noted challenges in accessing survivor-centered care, including the fact that providers multitasked during care.
Survivors said mental health services for survivors of sexual violence are often unavailable in their communities, due to closed facilities, missing staff, or infrastructure challenges.
Quality
Survivors frequently reported challenges related to the quality of services being offered. They shared their doubts regarding the skill level of health professionals on providing mental health services and how to engage with survivors of sexual violence. Survivors saw challenges in the implementation of existing policies and standards ensuring quality care in their areas.
Kenya has a clear obligation under national laws and policies to address these gaps and provide high quality, accessible, acceptable, and available mental health care. The Constitution of Kenya affirms that “every person has the right to the highest attainable standard of health.”[13] The Mental Health Amendment Act’s 2022 revisions state that survivors of sexual violence are entitled to access affordable mental health services in Kenyan health facilities.[14] The Sexual Offences Act Medical Regulations operationalize the provisions of the Sexual Offences Act and provide a legal foundation for access to no-cost post-rape care, which includes mental health services (i.e., counselling) for survivors of sexual violence.[15] The National Guidelines on Management of Sexual Violence in Kenya[16] provide guidance on the survivor-centered implementation of health services for survivors, including mental health services. This solid legal framework provides a robust platform from which Kenya’s national and local governments can implement existing laws to realize the right to mental health of survivors of sexual violence. Despite the strong domestic legal and policy landscape for the provision of mental health care for survivors of sexual violence, there is a gap in the implementation of these policies.
Finally, the government of Kenya, as a party to international human rights treaties and obligations – including the International Covenant on Economic, Social and Cultural Rights, the Convention on the Elimination of All Forms of Discrimination against Women, the African Charter on Human and Peoples’ Rights, and the Protocol to the African Charter on the Rights of Women in Africa (the Maputo Protocol) – is obligated to ensure that all sexual violence-related care (including mental health care) is provided in line with the AAAQ framework and should address obstacles to the realization of these standards.
Survivors perceived gaps in the availability, accessibility, acceptability, and quality of mental health services. They said there is minimal prioritization of mental health care services in general, and specifically of services targeting survivors of SGBV and other vulnerable groups.
Conclusion and Recommendations
This assessment not only deepened understanding of the perceptions of survivors of sexual violence about the challenges they face in accessing mental health services, but it also prioritized the engagement of survivors in advocating for change in their communities. This enables the results of this assessment to contribute to action and advocacy efforts. Finally, this assessment shows that Photovoice, as an example of a participatory research and evaluation method, can be a powerful tool to ensure that survivors of sexual violence can remain in the center of assessments, research, and evaluations conducted to understand their experiences.
Based on the assessment’s results, PHR and the Survivors of Sexual Violence Network in Kenya offer the following recommendations:
To all stakeholders, including national and county governments and civil society organizations:
▪ Ensure that measures are taken to engage survivors’ perspectives and ensure that their voices are included, listened to, and heard in processes to improve mental health services for survivors. This includes ensuring that survivors of sexual violence are able to engage at public meetings at the sub-county, city, national and other levels. Stakeholders must proactively engage survivor networks, such as the Survivors of Sexual Violence Network in Kenya, when developing laws, policies, and programs meant for survivors. Finally, stakeholders should leverage participatory methods to engage survivors to integrate survivor priorities in the design of polices and legislation.
▪ Engage in reparations and transitional justice processes to ensure the inclusion of mental health care and services for survivors of sexual violence, as part of survivor-centered and holistic reparations.
To the Nairobi City County Government:
▪ Prioritize the establishment of the Mental Health Council as per the provisions of the Mental Health Amendment Act. The council should include experts in mental health and representatives of survivors’ groups to ensure that the specific mental health needs of survivors of sexual violence are represented on the council. They should be required to maintain a register of all private mental health facilities operating within their counties and submit these to the Mental Health Board annually. They should also be mandated to inspect these facilities and report their findings to the Mental Health Board for remedial action that may be necessary.
▪ Allocate more financial resources to mental health service provision and increase the number of staff offering mental health services. Dedicate additional funding and conduct annual capacity development for all health care providers on the provision of mental health services to ensure all are equipped with the skills to provide trauma-informed, survivor-centered initial mental health support, forensic psychological documentation, and referrals as needed.
▪ Strengthen the integration of mental health service provision into routine and primary health care, including ensuring that primary health care providers can identify and refer survivors of sexual and gender-based violence (SGBV) to mental health services.
▪ Fully implement the National Guidelines on Management of Sexual Violence in Kenya at health facilities that provide post-rape care, with particular emphasis on provisions of the guidelines that enhance the survivor-centered aspects of mental health-related service delivery, including ensuring privacy.
▪ In line with the Sexual Offenses Act Medical Regulations and The Nairobi City County SGBV Management and Control Bill, allocate county health funds to guarantee no-cost post-rape care and affordable mental health care for priority populations.
▪ Ensure that mental health providers are available to provide services during the hours of clinic operation.
▪ Train and engage community mental health workers to offer appropriate first-line mental health services to and referrals for survivors of sexual violence. This should include new and formal programs with survivors’ networks to provide peer support and engagement with other survivors.
▪ Conduct public education campaigns to create awareness on the importance of mental health care, psychosocial support, and the mental health impacts of SGBV in order to address community level stigma, discrimination, and negative attitudes related to mental health care and treatment that prevent many survivors from accessing services. This should include dissemination of information on the mental health services that are available to survivors, which clinics offer mental health services, hours of operation, and which services are free of charge.
▪ Develop new programs to ensure mental health services are more accessible to survivors of sexual violence. This should be done by providing transportation or transportation stipends to ensure survivors can return for mandated follow-up counselling sessions. Develop programs to offer home-based, online, virtual, or phone-based counselling services or at the community level to reduce the physical, logistical, and financial barriers to accessing mental health services.
▪ Ensure that health facilities and locations for mental health services are accessible and user-friendly. Additionally, provide wheelchairs, ramps, and signs that indicate where facilitates are located, and update publicly available information about when service providers will be available to provide services.
▪ Ensure that the privacy of survivors of sexual violence seeking mental health is protected at all public facilities, in line with the National Guidelines on Management of Sexual Violence. This should include access to private and separated treatment rooms where survivors can access services without fear of disclosure or interruption.
To the Ministry of Health:
▪ Prioritize the provision of trauma-informed, survivor-centered mental health services for survivors of SGBV, including, specifically, mental health counseling and access to psychological assessments, where needed, to capture critical evidence of sexual violence.
▪ Further develop and implement guidelines and protocols for the health sector on the provision of comprehensive mental health services to SGBV survivors. Specifically, expedite the adoption of the rules and regulations that will operationalize the Mental Health Amendment Act 2022, including ensuring access to mental health care without discrimination.
▪ Design, fund, and implement comprehensive training, campaigns, and awareness-building on the importance of mental health care for survivors of sexual violence for all health care workers, as well the scope and nature of legal obligations and national and international standards on the provision of such care. Develop standardized training materials and continuous medical education courses for health care workers to provide survivor-centered, trauma-informed mental health services and psychosocial to support survivors of sexual violence. This training should be conducted simultaneously with the development/implementation of facility and community health protocols to support the management of SGBV survivors.
▪ Through the National Treasury, allocate resources to county governments for the training, recruitment, and deployment of well-trained mental health service providers.
▪ Ensure the availability of funds at the county level and undertake monitoring to ensure survivors can meaningfully access no-cost services for post-rape care, including psychological assessments and mental health care, as mandated by the Sexual Offenses Act Medical Regulations. Increase the budgetary allocation to mental health services to, at a minimum, the recommended WHO standards at the national level.
▪ Undertake and fund additional assessments, research, and data collection on the impact of sexual violence on survivors’ mental health to be used to increase the accessibility, availability, acceptability, and quality of mental health services for survivors of sexual violence.
▪ Implement accountability processes at the national and county levels to monitor and evaluate the provision of high-quality, acceptable, available, and accessible mental health care for survivors of SGBV, without discrimination, and provide redress and remedy where survivors face barriers in accessing such care, including investigations by the Kenya National Commission on Human Rights where there are suspected violations of rights related to the mental health care of survivors.
▪ Ensure targeted implementation of the existing laws, including the Constitution of Kenya (article 43) and the Mental Health Amendment Act, to ensure that the right to the highest attainable standard of health is realized.
To Donors:
▪ Continue to support survivor’s groups and programs that provide mental health care for survivors, including capacity development for service providers on mental health care, survivor-centered approaches, and psychological documentation.
▪ Support programs that use participatory approaches to engage survivors in assessments, research, and monitoring and evaluation.
To organizations conducting assessments, research, and monitoring and evaluation with survivors of sexual violence:
▪ Use participatory research and evaluation methods, such as Photovoice, to leverage their utility as powerful tools that ensure survivors of sexual violence remain in the center of assessment, research, and monitoring and evaluation conducted with the aim of understanding survivor experiences and producing recommendations that will result in changes in spaces that matter most to survivors.
Acknowledgements
This assessment was written by staff members of Physicians for Human Rights’ (PHR) Program on Sexual Violence in Conflict Zones, Thomas McHale, SM, deputy director, Suzanne Kidenda, senior program officer- Kenya, and Olivia Dupont, MPH, program manager; and Millicent Akinyi, Jane Alfayo, Mercy Etole, Grace Kamau, Beatrice Karore, Margaret Kinyua, Ashura Mciteka, Diana Mushiyi, Lorraine Ong’injo, and Bonila Sisia, members of the Survivors of Sexual Violence in Kenya Network.
The assessment benefitted from review by PHR staff, including Erika Dailey, MPhil, director of advocacy and policy, Christian De Vos, JD, PhD, director of research and investigations, Lindsey Green, MA, senior program officer, Karen Naimer, JD, LLM,
MA, director of programs, Naitore Nyamu-Mathenge, LLM, MA, Kenya head of office, Dr. Ranit Mishori, MD, MHS, FAAFP, senior medical advisor, Payal Shah, JD, director, Program on Sexual Violence in Conflict Zones, Kevin Short, deputy director of media and communications, and Saman Zia-Zarifi, JD, LLM, executive director. The assessment was strengthened through external review by Donna Shelley, MD, MPH. It was reviewed, edited, and prepared for publication by Claudia Rader, MS, PHR senior communications consultant, with assistance from Samantha Peck, PHR executive and program associate and board liaison.
PHR would like to thank Rutgers International for sharing curriculum materials that were adapted and used for Photovoice trainings in this project. This innovative assessment would not have been possible without the generous support of the Comic Relief & UK Aid Mental Health Programme.
Above all, PHR is grateful to partners from the Survivors of Sexual Violence in Kenya Network (SSVKenya) who shared their time, stories, and photographs with us, and for the partnership with SSVKenya, whose members continue to passionately represent the priorities of survivors in Kenya and beyond.
Citations and Endnotes
[1] “Facts and Figures: Ending Violence against Women,” UN Women – Headquarters, https://www.unwomen.org/en/what-we-do/ending-violence-against-women/facts-and-figures.
[2] This statistic only includes women and girls aged 15-19 who were usual members of (or slept at the night before) households sampled as part of the Kenya Demographic and Health survey, 2022.
[3] Kenya National Bureau of Statistics, Ministry of Health/Kenya, National AIDS Control Council/Kenya, Kenya Medical Research Institute, and National Council for Population and Development/Kenya, 2023, Kenya Demographic and Health Survey 2022, Rockville, MD, USA: Available at https://dhsprogram.com/pubs/pdf/PR143/PR143.pdf.
[4] “WHO Multi-Country Study on Women’s Health and Domestic Violence against Women,” n.d.
[5] Nikram Patel, Neerja Chowdhary, Atif Rahman, and Helen Verdeli, 2011, “Improving Access to Psychological Treatments: Lessons from Developing Countries,” Behaviour Research and Therapy 49 (9): 523–28. https://doi.org/10.1016/j.brat.2011.06.012.
[6] Survivor-collaborator quote, Data collection period October 28 – November 4, 2023.
[7] Survivor-collaborator quote, Data collection period October 28 – November 4, 2023.
[8] Survivor-collaborator quote, Data collection period October 28 – November 4, 2023.
[9] M. Candace Christensen, 2017, “Using Photovoice to Address Gender-Based Violence: A Qualitative Systematic Review,” Trauma, Violence, & Abuse, July, 152483801771774, https://doi.org/10.1177/1524838017717746.
[10] “Using Photovoice to Address Gender-Based Violence: A Qualitative Systematic Review.”
[11] Survivor-collaborator quote, Data collection period October 28 – November 4, 2023.
[12] Office of the UN High Commissioner for Human Rights, “The Right to Health Fact Sheet,” https://www.ohchr.org/Documents/Issues/ESCR/Health/RightToHealthWHOFS2.pdf.
[13] Constitution of Kenya 2010, Article 43(1). n.d., http://kenyalaw.org/kl/index.php?id=398.
[14] “The Mental Health Act,” Kenya, 2022.
[15] “Sexual Offences Act Medical (Treatment) Regulations,” Kenya, 2020.
[16] Nairobi, Ministry of Health, 2014, National Guidelines on Management of Sexual Violence in Kenya.
Through Our Lens: Visualizing Perceptions of Mental Health Services for Survivors of Sexual Violence in Kenya
Survivors of sexual violence in Kenya have the right to mental health care, yet services are widely lacking. For those who do attempt to find the mental health care they need, what do they experience?
This is the guiding prompt for images and reflections from survivors of sexual violence in Nairobi, Kenya. Using a participatory methodology called Photovoice, a group of women set out to document their journey to seek out and access mental health care. The resulting collection of images reveals significant gaps in the availability, accessibility, acceptability, and quality of mental health services being offered to survivors in Nairobi. Read more about this project
These photos ask us to consider how surviving sexual violence might change how a person looks at their community when using mental health services, where even daily scenes can take on new meaning: Crowded public transportation may induce anxiety; trash in a flooded lot evokes a sense of despair. For one survivor, even a malfunctioning streetlight is a reminder that women in Nairobi are at risk of attacks on the streets. Others described health facilities where survivors receive mental health services in areas that are not private, to show that even the services that are available do not always make survivors feel comfortable. In some of the images, survivors have recreated typical interactions, such as with strangers on the street, or in conversation with mental health professionals, to illustrate experiences of social stigma, isolation, and lack of privacy. Yet the images also convey hope. Women standing together in solidarity, or friends gathered together to talk about health care. Even smooth paving leading to a health clinic is an encouraging sign.
These survivors in Kenya were motivated to document issues important to them and their community. Taken together, their images serve as a reminder that survivors of sexual violence in Kenya have the right to mental health care, and the government of Kenya is obligated to provide it. Explore the galleries below or read the assessment “Voicing Our Plight: Using Photovoice to Assess Perceptions of Mental Health Services for Survivors of Sexual Violence in Kenya”
Ashura Mciteka
Beatice Karore
Bonila Sisia
Diana Mushiyi
Grace Kamau
Lorraine Ong’ijo
Millicent Akinyi
About the Project
In Kenya, 34 percent of women and girls aged 15-49 years surveyed have experienced physical violence at least once in their lifetime and 13 percent have experienced sexual violence, with many of these cases going unreported. SGBV has profound impacts on survivors’ physical and mental health, and access to mental health care is a major challenge for survivors of sexual violence.
Physicians for Human Rights’ Program on Sexual Violence in Conflict Zones began working in Kenya in 2011 to confront impunity for sexual violence committed during the unrest that followed the 2007 national elections. From 2020 to 2022, PHR worked with partners, including the Survivors of Sexual Violence Network in Kenya (SSVKenya) convened by the Wangu Kanja Foundation, to address challenges faced by survivors. These included medical-legal documentation of the mental health impacts of sexual violence and access to quality mental health services in Kenya.
The project, supported by the Comic Relief & UK Aid Mental Health Programme, aimed to enhance the capacities of health professionals and institutions in Kenya to provide post-rape mental health care and to forensically document the mental health impacts of sexual violence, as well as to strengthen the legal and policy framework on mental health care in Kenya.
This assessment arose out of PHR’s interest in understanding the impact of these interventions and related advocacy from the perspective of survivors of sexual violence, themselves. To ensure the voices of survivors remained at the heart of the assessment, PHR partnered with SSVKenya, an advocacy coalition comprised of survivors of sexual violence in Kenya.
Submission from PHR and the Cardozo Law Institute in Holocaust and Human Rights on International Criminal Court Office of the Prosecutor’s Policy on Children
Physicians for Human Rights (PHR) and the Cardozo Law Institute in Holocaust and Human Rights (CLIHHR) are pleased to provide this submission in response to the International Criminal Court (ICC) Office of the Prosecutor’s (OTP) call for suggested changes to build upon, and renew, the 2016 OTP Policy on Children. As organizations committed to addressing sexual and gender based crimes (SGBC) faced by children, PHR and CLIHHR offer this submission to suggest how the Policy on Children can be further developed to articulate key principles in addressing crimes occurring at the intersection of age and gender, and to incorporate practical tools, international standards, and reference materials to implement these principles in practice.
Human Rights Must Guide Pandemic Responses: 7 Lessons from COVID-19
Today marks a new chapter in the fight against COVID-19, as the Public Health Emergency (PHE) expires in the United States. Similarly, on May 5, 2023, the World Health Organization (WHO) announced the end of the Public Health Emergency of International Concern, downgrading COVID-19 from an emergency to an “ongoing health issue” with a need to focus on longterm management.
While we may be moving out of an acute, emergency phase of the pandemic, people are still dying from COVID-19 in staggeringly large numbers (more than 1000 deaths in the U.S. alone each week). As we can expect to see more incidents of infectious diseases in the future, we must not be complacent, especially when it comes to protecting vulnerable communities.
These transitions also represent a new chapter for Physicians for Human Rights (PHR). For the past year, I have helped lead PHR’s work around the COVID-19 pandemic. As the PHE comes to an end, I want to reflect on our engagement with the emergency over the last three years, to describe PHR’s hopes to continue its work going forward, and to highlight lessons to take forward in preparation for the inevitable next pandemic.
1. Vaccines saved lives. Vaccine equity would have saved even more.
The global bio-pharmacological response to COVID-19 was extraordinary, with tests, treatments and vaccines made at record speeds. International scientific information-sharing and collaboration among scientists, researchers, and health experts were likewise unprecedented. However, nationalism and vaccine hoarding led to many preventable deaths, widened inequities, and prolonged the pandemic.
PHR underscores the importance of centering human rights and equity in both pandemic response and any public health emergency. At the heart of vaccine inequity lies decades of underinvestment in global health and health infrastructure and a general lack of available or affordable access to pharmacotherapies and technologies.
PHR has continuously worked to highlight vaccine equity through various forms of advocacy including letters, data, webinars, press releases, and calls for accountability, as well as working to ensure that marginalized communities – such as those in immigration detention – are included in vaccine allocation and rollout. We joined other organizations calling for waiving intellectual property rules and urging the World Trade Organization to ease patents for COVID-19 tests and treatments. PHR has closely followed the Pandemic Accord (WHO CA+) negotiations and welcomes the inclusion and ongoing discussion of intellectual property, publicly funded goods, and the human rights responsibilities of governments and institutions. At the 77th World Health Assembly in May 2024 we hope to see an accord that has been strengthened rather than weakened, and one that creates a mechanism that protects the right to life for everyone, everywhere.
2. Protecting communities begins with protecting health workers.
In the early days of the pandemic, health workers throughout the world faced enormous challenges responding to the pandemic in clinical settings and at home. Health workers have faced verbal and physical abuse, stigmatization, the scourge of pervasive dis-misinformation, all while struggling to protect themselves both physically and mentally. From lacking adequate personal protective equipment, to needing greater support to combat burnout and increase their resilience, health workers have been tested like never before. PHR has advocated to support and uplift the voices of health workers through research, collaboration, resources, toolkits, and guidance both in the United States and internationally.
Protecting health workers and public health officials must be a core feature of preparing health systems for future emergencies. It is clear that if we cannot protect health workers and uplift their expertise, no one is safe.
3. Health and social impacts fall disproportionately on historically marginalized communities.
Throughout the world, the COVID-19 pandemic spotlighted and worsened existing inequities in access to health and demonstrated persistent threats to international human rights, including the right to equality and non-discrimination, the right to life, and the right to free movement. Understanding the unequal burdens and violations of human rights that have disproportionately impacted certain groups is vital and necessary.
Fear around COVID-19 helped fuel racism, discrimination and xenophobia globally. People of color, immigrants and undocumented workers – all of whom are often overrepresented in public-facing, “essential” jobs – were more likely to be exposed to COVID-19. Similarly, they were disproportionately impacted by inadequate safety net services, poor access to paid sick leave, and unaffordable or inaccessible health. We have seen how governments can weaponize health emergencies against ethnic minorities, refugees and asylum seekers, and impose unnecessary and disproportional limits on travel and border crossing.
In the United States, under the guise of public health, an order known as Title 42 allowed the government to expel children and adults seeking refuge in the US, despite the lack of scientific evidence to support it. PHR has advocated against this rule since it’s implementation and has filed several amicus briefs in federal courts. PHR also studied the impact of expulsions on health and human rights, rallied thousands of medical professionals, repeatedly called for an end to border expulsions, and continuously condemned the ongoing use of Title 42 expulsions. As Title 42 expires today, along with the Public Health Emergency, PHR will continue to monitor the impact of new Biden Administration policies on those seeking asylum. Public health cannot be weaponized to serve political agendas.
4. Misinformation and disinformation is deadly.
The world experienced a flood of constant COVID-19 mis- and disinformation, leading to health harms, erosion of public trust in science, and political battles over public health For example, areas of the United States exposed to television programming that downplayed the severity of the pandemic saw greater numbers of cases and deaths, likely because people ignored or dismissed public health recommendations. A recent analysis found that across the United States, and between January 2021 and April 2022, there were at least 318,000 vaccine-preventable COVID-19 deaths.
Scientists and health workers are important and trustworthy voices; they must be protected whenever navigating any pandemic or public health emergency. Mis- and disinformation attacked the integrity of health workers. In response, PHR has worked to empower physicians and health workers to fight back against health conspiracies. We have publicly supported empowering state medical boards to take action and discipline physicians who undermine public health and endanger their communities.
5. Civil society remains underrepresented at decision making tables.
Civil society organizations (CSOs) are crucial voices for representing the needs of communities and ensuring inclusion and accountability; they also have some of the most experience in advancing social protection and the application of public health measures. These valuable voices were underrepresented during the world’s COVID-19 response and continue to be inadequately engaged in preparedness and prevention discussions.
PHR has called for ongoing and additional inclusion of CSOs in the WHO Pandemic Accord. PHR has advocated for voices of civil society through open letters on participation and key priorities, engagement in high-level meetings, and a more holistic lens centering human rights at the United Nations General Assembly, with partners at the People’s Vaccine Alliance and The Civil Society Alliance.
6. COVID-19 fueled a “parallel pandemic” of gender-based violence.
Sheltering in place came with a rise of domestic and intimate partner violence globally, especially affecting women and children. The United Nations estimated that “6 months of lockdowns could result in an additional 31 million cases of gender-based violence.”
PHR has explored the impact of COVID-19 on clinical care and services for sexual and gender-based violence in the United Kingdom and Kenya and called for health worker education, health system responsibility, and multisectoral collaboration. We have likewise explored the unique challenges of navigating women’s health services during the pandemic, and how particular communities are impacted, including refugee communities and those living in conflict zones.
Future pandemic and public health emergency responses need to adopt a more robust gender lens. Sexual and gender-based violence services must be deemed essential, alongside comprehensive family planning and reproductive services.
7. Accountability is vital to address future pandemics.
To genuinely participate in adequate preparedness, prevention and response, governments, institutions, and organizations must critically review and evaluate decisions made during COVID-19 and be transparent about their findings.
PHR has sought to improve state accountability for inadequate COVID-19 responses by joining partner organizations in calling on global leaders to pledge that the mistakes of this pandemic not be repeated. To that end, PHR has supported the strategic litigation of the Open Society Justice Initiative, which recently filed a complaint before the European Committee of Social Rights (ECSR) against Bulgaria for failing to prohibit discrimination and failing to protect health during their COVID-19 vaccination rollout.
Governments, global health organizations and health-related funders have a duty and moral imperative to engage wholeheartedly in prevention and preparedness, and to uphold human rights in the process.
No One Could Say: Accessing Emergency Obstetrics Information as a Prospective Prenatal Patient in Post-Roe Oklahoma
Executive Summary
In the wake of the 2022 U.S. Supreme Court decision in Dobbs v. Jackson Women’s Health Organization, Oklahoma residents are currently living under three overlapping and inconsistent state abortion bans that, if violated, impose severe civil and criminal penalties on health care providers. Exceptions to these new laws, enacted around the Supreme Court’s overturning of its 1973 ruling in Roe v. Wade, are extremely limited and confusing to health professionals and potential patients alike. Because the exceptions drafted by legislators are often conflicting and use non-medical terminology, they sow confusion around what kinds of care and procedures health care providers can legally offer when a pregnancy threatens a person’s health or life. These challenges, combined with the significant penalties under these bans, constitute a situation of “dual loyalty”: health professionals are forced to balance their obligation to provide ethical, high-quality medical care against the threat of legal and professional sanctions. The decision to provide emergency medical care risks becoming a legal question – determined by lawyers – rather than a question of clinical judgment and the duty of care to the patient – determined by health care professionals.
In light of the extensive anti-abortion legal framework newly in place in the state, Oklahoma offers an important insight into the potential effects of near-total abortion bans on pregnant patients and the clinicians who care for them. While bans such as Oklahoma’s have already severely limited access to abortion medication or procedures, reproductive justice advocates have raised concerns that it is especially unclear what care remains accessible in practice in cases of obstetric emergencies. Accordingly, Physicians for Human Rights (PHR), Oklahoma Call for Reproductive Justice (OCRJ), and the Center for Reproductive Rights (CRR) have examined Oklahoma as a case study to investigate two key questions:
- Do hospitals have policies and/or protocols that govern decision-making when pregnant people face medical emergencies, and are pregnant people in Oklahoma able to receive information on these policies, if they do exist?
- If information is provided to prospective patients on hospital policies and/or protocols related to obstetric emergency care, what is the content and quality of that information?
To study these questions, PHR, OCRJ, and CRR used a “simulated patient” research methodology, in which research assistants posed as prospective patients and called hospitals that provide prenatal and peripartum care across the state of Oklahoma to ask questions related to emergency pregnancy care.
Not a single hospital in Oklahoma appeared to be able to articulate clear, consistent policies for emergency obstetric care that supported their clinicians’ ability to make decisions based solely on their clinical judgement and pregnant patients’ stated preferences and needs.
The results of this research are alarming. Not a single hospital in Oklahoma appeared to be able to articulate clear, consistent policies for emergency obstetric care that supported their clinicians’ ability to make decisions based solely on their clinical judgement and pregnant patients’ stated preferences and needs. Of the 34 out of 37 hospitals offering obstetric care across the state of Oklahoma that were reached, 65 percent (22 hospitals) were unable to provide information about procedures, policies, or support provided to doctors when the clinical decision is that it is necessary to terminate a pregnancy to save the life of a pregnant patient; only two hospitals described providing legal support for clinicians in such situations. In 14 cases (41 percent), hospital representatives provided unclear and/or incomplete answers about whether doctors require approval to perform a medically necessary abortion. Three hospitals indicated that they have policies for these situations but refused to share any information about them; four stated they have approval processes that clinicians must go through if they deem it necessary to terminate a pregnancy; and three stated that their hospitals do not provide abortions at all. (Oklahoma hospitals that are affiliated with an Indigenous nation were excluded from the study; because they operate under federal oversight, it is unclear how the Oklahoma bans impact them.) Some examples of the information the simulated patients received include:
- One hospital representative claimed: “If the situation is truly life-threatening, decisions will be made,” without explaining how those decisions would be made or by whom.
- Another hospital representative stated that, “[i]t is tricky because of state laws, but we will not let the mom die.”
- In one circumstance, the caller was told that a pregnant patient’s body would be used as an “incubator” to carry the baby as long as possible.
- At one hospital, a staff member put the simulated caller on hold and, after consulting with a hospital physician, told the caller, “Nowhere in the state of Oklahoma can you get an abortion for any reason,” even though the bans have exceptions.
In sum, in response to questioning, hospitals provided opaque, contradictory, and incorrect information about when an abortion is available; lacked clarity on criteria and approval processes for abortions; and offered little reassurance to patients that their survival would be prioritized or that their perspectives would be considered.
Hospitals provided opaque, contradictory, and incorrect information about when an abortion is available; lacked clarity on criteria and approval processes for abortions; and offered little reassurance to patients that their survival would be prioritized or that their perspectives would be considered.
The study’s findings demonstrate that despite apparently good-faith efforts from most hospital representatives, callers could not access clear and accurate information about the care they would receive if facing a pregnancy-related medical emergency at any given institution. Moreover, the information they received was often confusing – at some hospitals, callers received conflicting information from separate staff within the same hospital. These findings raise grave concerns about the ability of a pregnant person in Oklahoma – and the other 12 states with similar, near-total abortion bans – to receive clear, sufficient, and necessary information to make informed decisions about their medical care, as well as the ability of such patients to receive medically-necessary treatment. Callers also found that some hospital administrations, in an effort to comply with state laws, imposed restrictive policies on medical personnel that would impede their ability to provide prompt and effective care for pregnant patients with medical emergencies, including in cases of miscarriage.
One hospital representative claimed: “If the situation is truly life-threatening, decisions will be made,” without explaining how those decisions would be made or by whom. In one circumstance, the caller was told that a pregnant patient’s body would be used as an “incubator” to carry the baby as long as possible.
Health care providers face a similarly untenable situation under the current abortion bans. The criminalization of abortion denies access to abortion for pregnant people under most circumstances, and narrow exceptions such as “only to save the life” of the pregnant patient lead to confusion, uncertainty, and fear, both for pregnant people and for the hospitals and health care providers that care for them. Clinicians face severe criminal and civil penalties, such as the loss of their medical licenses and long prison sentences, if prosecutors and state legislators disagree with their medical decision-making. In light of these obstacles, pregnant people are faced with the frightening possibility that they will be unable to receive science-informed, patient-centered, and ethical medical care should they face an obstetric emergency.
These results reflect how Oklahoma’s abortion bans threaten the health and well-being of pregnant people and violate their human rights. These violations include individuals’ rights to life, health, equality, information, freedom from torture and ill-treatment, and to exercise reproductive autonomy. These findings further affirm what has been recognized by the World Health Organization: that the criminalization and penalization of abortion care – even with an exception for medical necessity – is fundamentally inconsistent with evidence-based, ethical, and patient-centered health care.
Oklahoma’s abortion bans threaten the health and well-being of pregnant people and violate their human rights.
Given these findings, PHR, OCRJ, and CRR make the following topline recommendations: (full recommendations can be found below)
To the Oklahoma Legislature:
- Repeal Oklahoma’s abortion bans and decriminalize abortion.
- Ensure that health care services for pregnant people and all Oklahomans are accessible and of good quality.
To Oklahoma’s Hospitals and Health Care Professionals:
- Speak out against laws criminalizing abortion or otherwise restricting access to abortions, including during obstetric emergencies.
- Build knowledge and awareness of professional recommendations and guidance for providing abortion services.
To State and National Medical Associations:
- Publicly condemn abortion bans and continue to speak out against the dual loyalty impacts of abortion bans, including citing evidence of how such laws undermine ethical obligations and professional duties of care.
To the Federal Government:
- Enact and implement national laws and policies that ensure rights and remove barriers to abortion care and maternal health care.

Introduction
In June 2022, the U.S. Supreme Court issued its decision in Dobbs v. Jackson Women’s Health Organization overturning almost 50 years of legal precedent and eliminating the federal constitutional right to abortion. This decision marked the first time in American history that the Supreme Court took away a right it had recognized as fundamental to personal liberty. As U.S. Attorney General Merrick Garland noted, abortion has been “an essential component of women’s liberty for half a century – a right that has safeguarded women’s ability to participate fully and equally in society.”[1]
Oklahoma was one of many states that sought to ban abortion in the lead-up to – and in the wake of – the Dobbs decision. It now has three overlapping abortion bans in effect, each with different elements and exceptions. A fourth ban with criminal penalties was enacted in 2022, but that law was struck down by the Oklahoma Supreme Court in March 2023. Providing someone with an abortion or assisting them in accessing an abortion in Oklahoma remains illegal, except in narrowly and ambiguously defined medical emergencies and circumstances that threaten a pregnant person’s life.[2] State legislators in Oklahoma continued to push legislation in 2023 that creates further legal risk for those involved in receiving and providing care for pregnant people in cases of emergencies.
In light of the many anti-abortion laws enacted in recent years in the state, Oklahoma offers an important view into the potential effects of near-total abortion bans on pregnant patients and the clinicians who care for them, both in Oklahoma and in other states with similar bans. Using a “simulated patient” research methodology, this study examined whether pregnant people could access information about the care they might receive at Oklahoman hospitals that provide prenatal and peripartum care, should they face a medical emergency – and, if they could, the quality and clarity of that information.

The Effect of Dobbs on Abortions Provided Due to a Medical Emergency
In the wake of the Dobbs decision, a number of states swiftly began instituting or enforcing laws that nearly or entirely ban abortion with narrow exceptions, many with criminal penalties for health professionals who provide abortion care. As of April 2023, 13 states have instituted and are enforcing abortion bans.[3] For example, Arkansas bans abortions at all stages of pregnancy, with no exemptions except to “save the life” of a pregnant person.[4] Mississippi similarly bans abortion with narrow exceptions to “save the life” of a pregnant person or in cases of rape or incest that are reported to law enforcement.[5] South Dakota bans abortions with exceptions to “preserve the life” of a pregnant person.[6] The impact of these laws will fall hardest on people who already face discriminatory obstacles to health care: Black, Indigenous, and other people of color, people with disabilities, people in rural areas, young people, undocumented people, and those with limited financial resources.[7]
Many of these states’ laws contain language that does not reflect precise or accurate medical terminology, particularly in describing valid legal exemptions to the bans. Of particular concern, as of February 21, 2023, four out of the 13 states with abortion bans include exemptions phrased along the lines of, “except when necessary to save the life of the mother,” with no further detail, explanation, or other exemptions.[8] Four other states use this language and add only one additional exception written along the lines of, “to prevent severe, permanent damage to major organs or bodily functions.”[9]
In practice, the language used for exceptions to abortion bans is open to interpretation. This may seem like a positive measure – giving deference to clinicians in applying laws. However, against a backdrop of criminalization and inconsistent exceptions that do not utilize medical language, such exceptions only sow more fear and confusion and potentially make clinicians reluctant to take steps to provide necessary medical care to patients.[10] For instance, what circumstances or indicators of medical severity qualify as an emergency that threatens a pregnant person’s life? How imminent or severe must the threat be? What are appropriate mechanisms and policies that health systems must enact to provide support, guidance, and legal protection for health professionals faced with these time-sensitive and critical clinical decisions? To what extent are or should a patient’s own views and tolerance for risk be considered in such decision-making?
These narrow, vague exceptions to criminalization place medical professionals providing care for pregnant patients in the position of balancing their duty to provide ethical, high-quality medical care against the threat of legal and professional sanctions. In other words, physicians must weigh concerns for their patients’ health with the recognition that their actions in medical emergencies could leave them vulnerable to criminal charges, with potential penalties as severe as 15 years in prison, thousands of dollars in fines, and loss of their medical licenses. Such conflicts constitute dual loyalty, a situation in which health care workers “find their obligations to their patients in direct conflict with their obligations to a third party … that holds authority over them” – in this case, state governments.[11]
Physicians must weigh concerns for their patients’ health with the recognition that their actions in medical emergencies could leave them vulnerable to criminal charges, with potential penalties as severe as 15 years in prison, thousands of dollars in fines, and loss of their medical licenses.
This concern has quickly proven true. American Medical Association President Jack Resneck, Jr. has decried the “chaos” into which health care has been thrust since the Dobbs decision, describing physicians as “caught between good medicine and bad law,” struggling to “meet their ethical duties to patients’ health and well-being, while attempting to comply with reckless government interference in the practice of medicine that is dangerous to the health of … patients…. Physicians and other health care professionals must attempt to comply with vague, restrictive, complex, and conflicting state laws that interfere in the practice of medicine.”[12]
American Medical Association President Jack Resneck, Jr. has decried the “chaos” into which health care has been thrust since the Dobbs decision, describing physicians as “caught between good medicine and bad law.”
Providers have shared concerns about confusion related to medical emergencies and the incompatibility of various state abortion laws with caring for patients facing such emergencies. Tennessee has an abortion ban with no exceptions, although it allows providers to raise a defense in a prosecution that an abortion was medically necessary. Seven hundred doctors signed on to a letter calling on legislators to reconsider the ban for a variety of reasons, including because “it forces health care providers to balance appropriate medical care with the risk of criminal prosecution.”[13] Similarly, Louisiana doctors who are operating under several bans attested that “[f]ear of punishment aligned with lack of clarity on how this law will be enforced can lead to devastating consequences for Louisiana women as well as moral distress for the clinicians who care for them and have taken the Hippocratic oath to do no harm.”[14] Common pregnancy complications may present situations where providers are too cautious in providing necessary care because they are concerned that a patient is not sick enough, such as if a patient presents with preterm premature rupture of membranes (i.e., when the amniotic sac surrounding the fetus prematurely ruptures), potentially serious infections, or with other preterm complications that require emergency medical intervention and are likely to result in pregnancy loss or long-term harm to the pregnant person’s health and reproductive capacity.[15]
The bans also have concerning implications for the medical management of miscarriages (threatened, incomplete, or complete). It is estimated that up to 26 percent of pregnancies end in miscarriage, many of which require medical intervention to avoid health emergencies such as infection or hemorrhage.[16] Media reports reflect that the unclear language employed by many states in their abortion bans is causing confusion and hesitation among health professionals when handling miscarriages that require medical management, such as the surgical removal of a nonviable fetus and cases in which there is still fetal cardiac activity.[17] This is because treatments for miscarriage are the same as those used to provide an abortion.[18] These reports also demonstrate a growing sense of fear among patients about the care they might receive at health care facilities should they present with common symptoms such as bleeding or pain, as well as anxiety surrounding future pregnancies.
Indeed, prospective patients face the daunting task of trying to determine what these laws mean for the care they can expect to receive in hospitals in states with abortion bans. The answers to these crucial questions may vary considerably across health care institutions. Thus, pregnant people in these states struggle to access necessary information about how their own possible obstetric emergencies might be handled at different hospitals to determine their best options for maternity care, what treatment options are legal, and whether they can receive information in advance to better guide their decision-making.[19] Would a hospital they are considering require multiple layers of bureaucracy to secure approvals to terminate a pregnancy – such as oversight committees or requirements for second physicians to agree that their life is sufficiently at risk – that could create delays, leading to their death? Moreover, can patients trust the hospitals to support clinicians who prioritize their lives in the face of a life-threatening medical emergency? Without receiving clarity on these crucial questions, pregnant people struggle to make informed decisions about where to seek care.
To help answer these questions, Physicians for Human Rights (PHR), Oklahoma Call for Reproductive Justice (OCRJ), and the Center for Reproductive Rights (CRR) have examined Oklahoma as a case study to investigate two key questions:
- Do hospitals in Oklahoma have policies and/or protocols that govern decision-making when pregnant people face medical emergencies, and are pregnant people in Oklahoma able to receive information on these policies, if they do exist?
- If information is provided to prospective patients on hospital policies and/or protocols related to obstetric emergency care, what is the content and quality of that information?
The following report describes the research methodology for this study, its findings, relevant legal and ethical standards, and recommendations based on what the research revealed.
Legal Background
At the time of this writing, Oklahoma has three overlapping abortion bans (two civil and one criminal) in effect as well as a homicide statute that could be applied to the provision of abortion. A fourth ban with criminal penalties was enacted in 2022, but that law was struck down by the Oklahoma Supreme Court in March 2023. These laws have inconsistent prohibitions and penalties, resulting in a dangerous lack of clarity around their application. In particular, the exceptions in the laws permitting abortion in cases of medical emergencies conflict, which has resulted in significant confusion around when abortions are permitted in the face of a medical emergency.
On March 21, 2023, the Oklahoma Supreme Court issued a 5-4 decision upholding the constitutionality of Oklahoma’s 1910 pre-Roe ban on abortion but striking down a 2022 criminal ban on the grounds that its narrow medical exceptions provision violated the “inherent right of a pregnant woman [under the Oklahoma Constitution] to terminate her pregnancy when necessary to preserve her life.” The opinion did not address still-pending challenges to two other civil bans, which both include “medical emergency” language that was found to be unconstitutional in the Court’s decision. The Oklahoma Supreme Court stated that it “would define this inherent right to mean: a woman has an inherent right to choose to terminate her pregnancy if at any point in the pregnancy, the woman’s physician has determined to a reasonable degree of medical certainty or probability that the continuation of the pregnancy will endanger the woman’s life due to the pregnancy itself or due to a medical condition that the woman is either currently suffering from or likely to suffer from during the pregnancy. Absolute certainty is not required; however, mere possibility or speculation is insufficient.” This decision could ultimately provide greater comfort to health care providers treating patients experiencing emergent conditions, but given the other two civil bans still in effect (one of which has the same medical exception deemed insufficient by the Oklahoma Supreme Court), confusion is unlikely to be assuaged at present. At publication, it remains unclear how hospitals will react to the decision.
Legislators have not been able to articulate how these bans operate together. An investigative journalist contacted all 42 lead sponsors and cosponsors of the four recent abortion bans and found that none could “answer basic questions about the bans’ enforcement.”[20] Oklahoma’s attorney general acknowledged confusion about the application of these bans in guidance to law enforcement that was issued on August 31, 2022.[21] The guidance is not binding, and it does not clearly remedy the conflicts, nor does it address the two civil bans.[22]
The four recent abortion bans took effect one after another starting just before the Dobbs decision was released on June 24, 2022. First, Oklahoma enacted two abortion bans modeled after Texas S.B. 8, allowing private citizens to bring lawsuits against those who provide abortions or assist those seeking abortions. Then the state enacted two more abortion bans with criminal penalties. Three remain in effect:
- S.B. 1503 (“6-Week Civil Ban” or “Heartbeat Law,” effective May 3, 2022): The 6-Week Civil Ban prohibits physicians from “knowingly” providing an abortion after “detect[ing] a fetal heartbeat” or if the physician “failed to perform a test to detect a fetal heartbeat.” [23] The law creates a civil enforcement mechanism by which any person not affiliated with the state or local government “may bring a civil action against any person” who performs a prohibited abortion, “knowingly” aids or abets a prohibited abortion, or intends to engage in these activities.[24]
- H.B. 4327 (the “Total Civil Ban,” effective May 25, 2022): The Total Civil Ban shares a similar civil enforcement scheme with the 6-Week Civil Ban, but it applies from the moment of “fertilization.” [25]
- 21 Okla. Stat. § 861 (the “1910 Criminal Ban,” effective June 24, 2022): The 1910 Criminal Ban was an old law blocked after Roe v. Wade was decided, which was revived when “the Attorney General certifie[d] that … [t]he United States Supreme Court … overruled in whole or in part Roe … and … Casey.” [26] Oklahoma’s attorney general issued this certification on June 24, 2022, the same day Dobbs was decided. The statute prohibits an abortion at any point during a pregnancy.[27]
- S.B. 612 (the “2022 Criminal Ban,” struck down by the Oklahoma Supreme Court on March 21, 2023): The 2022 Criminal Ban prohibited abortion at any stage of pregnancy, with more extreme criminal penalties than the 1910 Criminal Ban.[28]
Oklahoma’s homicide statute could also be used to prosecute providers of abortion because the law considers the “killing of an unborn child” to be a homicide, punishable by up to life in prison.[29] Further, medical licensing boards are empowered to discipline clinicians and take action to suspend or revoke their licenses based on any violations of state law.[30]
Oklahoma’s homicide statute could also be used to prosecute providers of abortion because the law considers the “killing of an unborn child” to be a homicide, punishable by up to life in prison.
The resulting statutory framework includes inconsistent definitions, intent provisions, exceptions, and penalties (see table below).
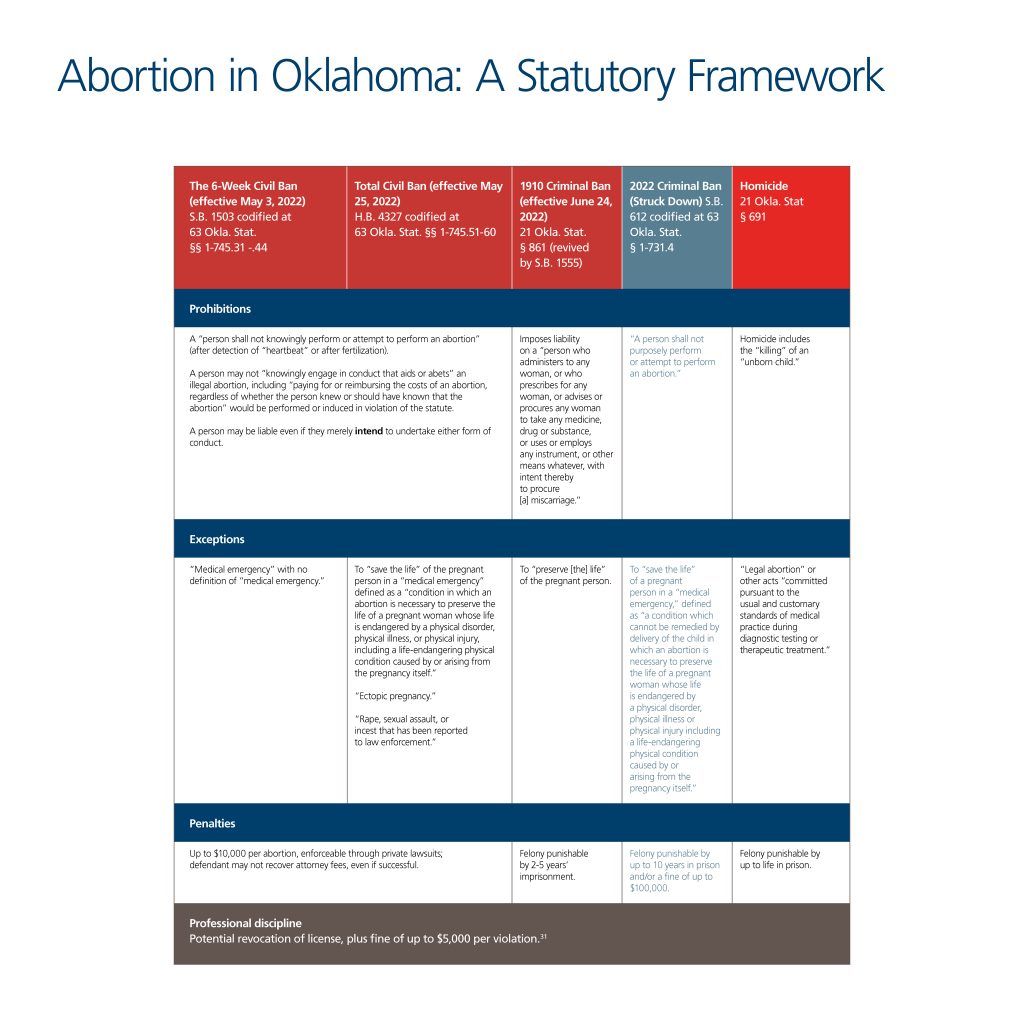
Understanding the scope and nature of permitted exceptions for abortion is particularly challenging under these laws. The Total Civil Ban permits abortion only when necessary to preserve a person’s “life in a medical emergency,” defined as a “condition in which an abortion is necessary to preserve the life of a pregnant woman whose life is endangered by a physical disorder, physical illness, or physical injury, including a life-endangering physical condition caused by or arising from the pregnancy itself,” although the 2022 Criminal Ban was struck down because of an almost identical “medical emergency” exception.[32]
The other abortion bans in effect, however, do not discuss exceptions based on specific medical emergencies. The 6-Week Civil Ban contains an exception for medical emergencies but does not define what counts as a medical emergency.[33] The 1910 Ban, which has now been upheld by the Oklahoma Supreme Court, similarly includes no mention of specific medical emergencies, as it only permits abortions to “preserve [the] life” of the pregnant person.[34] Meanwhile, Oklahoma’s homicide statute criminalizes the killing of an “unborn child,” except for a “legal abortion” or other acts “committed pursuant to the usual and customary standards of medical practice during diagnostic testing or therapeutic treatment.”[35] Further, the Total Civil Ban explicitly exempts care for an “ectopic pregnancy” and allows abortion for pregnancies resulting from “rape, sexual assault, or incest that has been reported to law enforcement.”[36] None of the other bans expressly carves out such exemptions.
Under these provisions, physicians cannot know when they are legally permitted to end a pregnancy. In a “medical emergency” that merely “endangers” the life of the patient, must they wait until the patient’s life is in immediate jeopardy? What criteria must be used to determine that this threshold is met? For example, are ectopic pregnancies (a dangerous medical condition in which a fertilized egg implants outside of the uterine cavity, typically in a fallopian tube) clearly exempted? The Oklahoma bans fail to answer these vital questions.

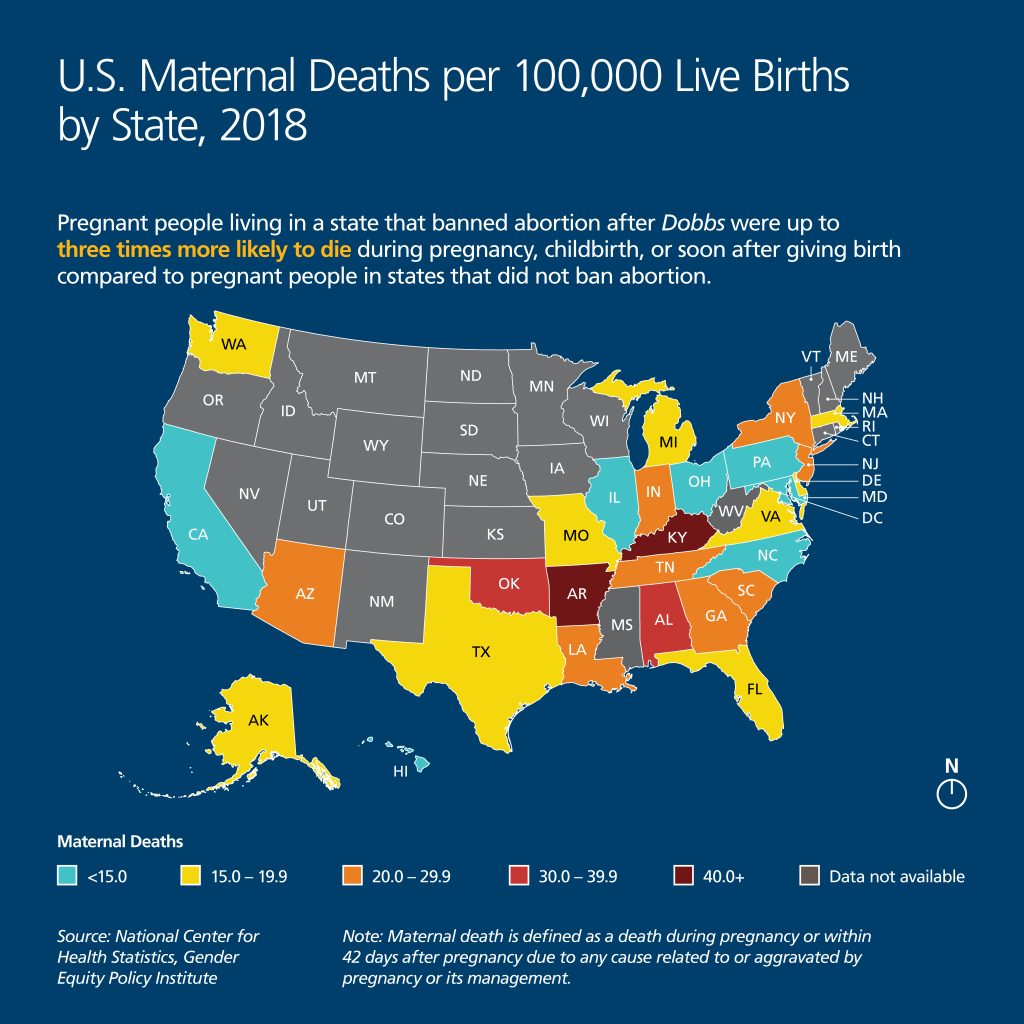
Impacts on Health
The medical literature is clear that criminal abortion bans are linked to a range of negative physical and mental health outcomes for pregnant people, in the United States and around the world. The unworkability of even an exception in the context of medical emergencies particularly implicates maternal mortality and morbidity. Constraining physicians from providing necessary care in medical emergencies is extremely dangerous for patients. The United States already has the highest maternal mortality rate of all high-income countries, with the U.S. maternal death rate further increasing over the COVID-19 pandemic, from 20.1 deaths per 100,000 live births in 2019, to 23.8 in 2020, to 32.9 in 2021.[37] Moreover, “For every U.S. woman who dies as a consequence of pregnancy or childbirth, up to 70 suffer hemorrhages, organ failure or other significant complications, amounting to more than 1 percent of all births,” according to data from ProPublica and NPR.[38] This crisis in U.S. maternal health outcomes disproportionately impacts people from Black, Indigenous, and low-income communities, who consistently face the greatest risks during their prenatal, pregnancy, childbirth, and postpartum phases linked to historic discrimination and inadequate access to quality health care. [39]
The medical literature is clear that criminal abortion bans are linked to a range of negative physical and mental health outcomes for pregnant people, in the United States and around the world. Constraining physicians from providing necessary care in medical emergencies is extremely dangerous for patients.

According to the Gender Equity Policy Institute, pregnant people living in a state that banned abortion after Dobbs were up to three times more likely to die during pregnancy, childbirth, or soon after giving birth compared to pregnant people in states that did not ban abortion.[40] This continues a trend in the United States wherein states that support reproductive health services, including by expanding Medicaid and supporting access to abortion and contraception, have lower maternal mortality rates than states that have restricted access to reproductive health care.[41] These disparities will likely increase as abortion bans continue to take effect around the country, with people of color among the most likely to suffer.[42]
Oklahoma exemplifies this alarming trend. Black and Indigenous residents of Oklahoma face significantly higher rates of maternal mortality than white residents. Moreover, Oklahoma “persistently ranks among the states with the worst rates” of maternal deaths in the United States, and maternal deaths in Oklahoma have “increased in recent years.”[43] According to the Oklahoma State Department of Health, from 2004 to 2018, Black pregnant women in Oklahoma suffered “more than 2.5 times the rate of deaths compared to the white population,” a statistic the Oklahoma Maternal Mortality Review Committee called an “alarming disparity.”[44] The Department further concluded that Indigenous pregnant women in Oklahoma “have experienced up to 1.5 times the rate of deaths when compared to white women over the years.”[45]
According to the Gender Equity Policy Institute, pregnant people living in a state that banned abortion after Dobbs were up to three times more likely to die during pregnancy, childbirth, or soon after giving birth compared to pregnant people in states that did not ban abortion.
Methodology
The findings of this report are based on a “simulated patient” research methodology, in which research assistants posed as prospective patients and called hospitals that provide prenatal and peripartum care across the state of Oklahoma to ask questions related to emergency pregnancy care.[46] The value of this methodology is its ability to elicit realistic responses from staff, akin to how they would behave when dealing with an actual patient, thus avoiding the social desirability biases associated with self-reporting.[47] These methods have been used successfully in multiple studies of hospital practices and have been deemed scientifically and ethically sound.[48] This study was reviewed and deemed exempt from U.S. requirements for human subjects research by Physicians for Human Rights’ (PHR’s) Ethics Review Board (ERB).[49]
Two PHR research interns and one staff member were trained and used a standard script to call all hospitals in the state listed as offering labor and delivery services. Presenting themselves as prospective maternity patients choosing which hospital to go to for prenatal and peripartum care, they requested information about each hospital’s policies and procedures that would guide decision-making in: 1) cases of medical emergencies, where their life could be at risk if a pregnancy with a viable fetus were not terminated; and 2) cases of miscarriage that require procedures both when there is and when there is not fetal cardiac activity.
To identify hospitals to be called, the research team reviewed several databases of all registered hospitals in Oklahoma maintained by the Oklahoma Hospital Association and by OfficialUSA.com.[50] The team then examined each hospital’s website to identify facilities that offer prenatal and peripartum services. In obstetric emergencies, hospitals’ obstetrics and labor and delivery clinical teams and departments are typically where difficult decisions about what constitutes “medically necessary” abortions are made and where such procedures are eventually carried out. From the review of each hospital’s website, the research team identified 41 facilities providing labor and delivery services in Oklahoma.
Since a prospective patient would likely first seek information from hospital websites, staff reviewed each hospital’s website in October 2022 for information on care in cases of potential miscarriage and medical emergencies during pregnancy. Two hospital websites described surgical procedures to remove ectopic pregnancies. No hospital website discussed care provided in other cases of medical emergency that could threaten the pregnant person’s life, and no hospital website described possible procedures or other treatment in cases of a potential miscarriage.
Staff members then built profiles for each of the 41 identified hospitals, categorizing them according to their religious affiliation, academic affiliation, size, association with an Indigenous nation, and geography. The four identified hospitals affiliated with an Indigenous nation were not included in the calls because it is currently unclear what the legal effects of Oklahoma’s bans are within these facilities, given that the Indian Health Service, which operates them, is under federal rather than state oversight (these facilities are also affected by the Hyde Amendment).[51] Thus, a total of 37 hospitals were called during the months of November and December 2022.
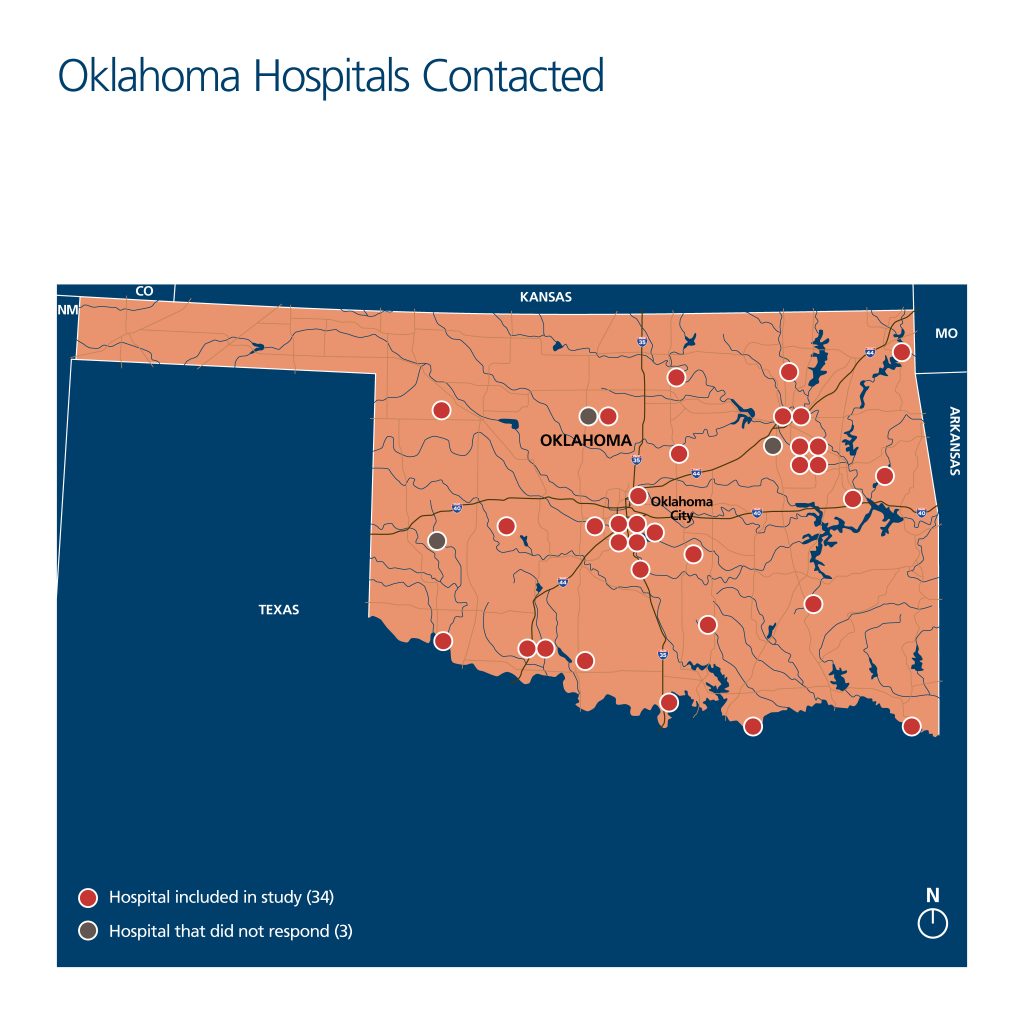

The simulated patients were assigned specific regions of the state to call (east, north, central, south, west), with a greater distribution of hospitals in Oklahoma’s central and northeastern regions. Each was trained to use a caller script and standardized note-taking sheet but was encouraged to alter the language and cadence of the questions, in the interest of appearing as realistic as possible and as individual conversations warranted. Each caller introduced herself under the following identity: a 36-year-old, highly educated, affluent, married woman with mild pre-existing conditions who had recently moved to Oklahoma.[55] The researchers stated that this was their first pregnancy and that they were currently six weeks pregnant. Callers used their real first names and a fictional last name in conversations and were provided an email address and the name of a universally accepted insurance plan (Blue Preferred PPO) to give hospital staffers if requested. If asked about their ethnicity, the research assistants were instructed to give their real backgrounds; all three callers were white women. Lastly, if callers were asked about their place of residence, all explained that they lived near the hospital called.
Written notes from the calls were kept on a standardized form. When relevant, the researchers wrote down verbatim quotes from hospital staff; however, none of the calls were recorded. Personal cell phones were used to make all calls.
During the calls, simulated patients requested to be informed about hospital policies that guided decision-making processes for “medically necessary” abortions to save the life of a pregnant patient and about the internal approval processes, if any, for conducting these procedures. The caller initially asked general questions about the hospital facility, such as if the hospital offered private delivery rooms, before shifting to more specific questions about the hospital’s guidelines in cases where an abortion might be required to save the life of the pregnant patient. As a pregnant person who recently moved to Oklahoma with her spouse, each caller’s questions were meant to convey a relatively informed patient’s concerns about how state-level abortion bans might affect the care they would receive in the case of a medical emergency, particularly given the existence of pre-existing, if routine, conditions.
In all calls, the simulated prospective patients requested to be connected to a qualified hospital representative who could answer their questions about care options during pregnancy. When hospital staffers provided vague or unclear explanations of hospital policies, callers gently probed for further clarification and, when necessary, requested to speak to another hospital employee who might have more complete information. If their efforts to speak to someone knowledgeable about hospital policies were unsuccessful during the call, the caller would thank the staff member, hang up, and call again later. Calls were considered complete if the callers were able to receive an answer about hospital policies or lack thereof from a member of the staff. If the initial call was inconclusive, the researchers would call hospitals back up to two more times before concluding the case. When a hospital provided information about its policies and guidelines for clinicians (or the lack thereof), verbally or through written communication, this was considered a “complete” call, and the call sheet was finalized. As discussed below, researchers were able to conduct “complete” calls with 34 Oklahoma hospitals.
Each completed call lasted approximately 15 minutes, with all efforts made to minimize call time so as not to burden hospital staff. If the hospital offered to set up an in-person or virtual appointment, the caller would decline the offer. All notes taken by the callers were de-identified and were stored on a password-protected server, accessed only by study staff associated with PHR. Hospitals were anonymized in these documents and for the report, using internally designated hospital IDs.
Of the 37 hospitals called, the callers reached staff who were able to talk about their policies at 34 facilities (92 percent response rate). At three hospitals, callers were transferred to appropriate representatives who never picked up, even after multiple attempts. There were no common characteristics among these three hospitals. For this reason, the universe of data for this report is the 34 Oklahoma hospitals where researchers were able to conduct a “complete” call.
At 23 hospitals (68 percent), the caller’s questions about hospital policies were answered in the first phone call. However, second or third calls were sometimes required because calls were dropped unexpectedly, staff did not initially answer the phone, or the callers had not received clear or conclusive answers in the first attempt. The callers were able to receive answers from eight hospitals (23 percent) after the second call and three (nine percent) after the third call. At all hospitals, the callers were referred to the labor and delivery unit/department or its equivalent. At six hospitals (approximately 18 percent), the callers spoke directly with a nurse.
Limitations
Four limitations to the “simulated patient” methodology and research design are worth noting. First, to the extent that any hospital staff members doubted the simulated callers’ identities, the responses they gave may have been incomplete or otherwise failed to disclose relevant information. There was no indication that hospital staff had such doubts, but it is a possibility.
Second, interactions with frontline staff and clinicians in these calls may or may not accurately reflect internal hospital policies or procedures, as this would depend upon the specific knowledge of the individual(s) spoken to. For all completed calls, the callers always spoke directly with labor and delivery ward staff members, while at six hospitals they were referred to speak directly with nurses, and at several others, hospital staff consulted clinicians. Definitive conclusions therefore cannot be drawn about whether hospitals did in fact have policies and guidelines, nor about what the content of any such policies and guidelines might be. However, because the aim of the study was to assess whether a prospective patient could receive necessary information to help guide an informed decision about where to receive maternity care, the information gained by the callers, whether accurate or not, is representative of what prospective patients would likely receive if they sought this information themselves.
Third, the callers’ fictional profiles are not representative of people who stand to be most harmed by Oklahoma’s abortion bans: low-income people, Black and Indigenous people, and other people of color. According to the standard script, the callers held universally accepted insurance plans, demonstrated that they were well-informed about Oklahoma’s anti-abortion laws, and in many cases were quite assertive in seeking to receive answers to their questions, insisting on speaking to other hospital staff if the initial person answering the call did not know whether there were hospital policies relevant to the inquiries. The study, therefore, does not assess what responses hospitals would give to those who do not have health insurance (currently an estimated 16 percent of adults in Oklahoma), who have less comprehensive or widely accepted insurance plans and thus lack the option of seeking care at another hospital, who are less empowered or assertive, who have lower health or English literacy, or who are unaware of Oklahoma’s abortion laws.[56] Moreover, although they did not identify themselves by race or gender identity, the caller-researchers were cisgender white women. They therefore do not share the lived experience of those who face discrimination and other barriers in accessing health care and experience significant disparities in maternal health outcomes, including Black and Indigenous people or other people of color, gender-nonconforming or transgender people, migrants, and those with low health or English literacy.
Finally, because hospitals serving Indigenous populations were not included in the study, conclusions cannot be drawn about prospective patients’ ability to receive information from these hospitals about their internal policies. This is an important limitation, as Oklahoma’s Indigenous population, which constitutes almost 10 percent of the state’s total population, has disproportionately worse maternal, infant, and child health outcomes than white Oklahomans. Given these disparities, it will be important to closely monitor the post-Dobbs maternal mortality and morbidity outcomes for Indigenous communities.
Notwithstanding these limitations, the results are meaningful. The fictional profile of the callers served the intended purpose of the study. That profile was chosen to ensure that results reflect the highest level of transparency a hospital would offer to prospective patients who request information to help determine where – among multiple options available to them – they would like to receive maternity care.
Overview of Findings
Staff members at most hospitals contacted demonstrated a willingness to talk with the simulated prospective patients about their concerns and sought to reassure the callers that they would still receive a high level of care under the new abortion laws. However, not a single hospital appeared to be able to articulate clear, consistent policies for emergency obstetric care that supported their clinicians’ ability to make decisions based solely on their clinical judgement and pregnant patients’ stated preferences and needs. At most hospitals, representatives were unable to tell the callers whether there was an approval process or any other guidelines to help clinicians determine that a pregnancy must be terminated to save the life of the patient, and they were similarly unable to describe what miscarriage management services were available to patients. In a few outlier cases, representatives explained that their hospitals had instituted such policies but refused to provide this information, in some cases citing an inability to share material with those outside of the hospital system, and in others offering no explanation. And in several hospitals, different representatives provided contradictory information about hospital policies and/or incorrect information about Oklahoma’s abortion laws.
Not a single hospital appeared to be able to articulate clear, consistent policies for emergency obstetric care that supported their clinicians’ ability to make decisions based solely on their clinical judgement and pregnant patients’ stated preferences and needs.
Callers received confusing and at times conflicting information about what would constitute a medical emergency and who could decide whether the emergency warranted terminating a pregnancy. Most hospitals reported that it is up to the treating doctors to make determinations about what constitutes a medical emergency where the pregnant person’s life is at risk. It was not clear, however, whether physicians are given guidance and legal support, nor whether they are required to complete certain procedures when they determine that a medical emergency exists that necessitates terminating a viable pregnancy. One hospital representative’s response exemplified the lack of clarity and transparency during the calls by claiming, “If the situation is truly life-threatening, decisions will be made,” without explaining what qualifies as “life-threatening,” how those decisions would be made, or by whom. At several hospitals, representatives explained that if a physician diagnoses a patient as experiencing a medical emergency that places the patient’s life at risk and requires an abortion, the physician must wait to receive approval from other entities – such as an ethics committee or a second physician – before terminating the pregnancy, raising concerns about the risk of possible harmful or even fatal delays.
The callers also received little clarity about how hospital administrations advise medical personnel to prioritize patient input, safety, and medical ethics during medical emergencies. In calls with most hospitals, no assurance was provided that the simulated patient would have a role in decision-making about pregnancy termination in medical emergencies where their life could be at risk. At one hospital, the caller was told, “You get a voice, but doctors make the final decision.” Moreover, at most hospitals, the callers were not provided reassurance that the pregnant patient’s life would be prioritized in medical decision-making. One hospital representative assured the caller that, “Here, we care equally about both the mother and the fetus” but did not answer further questions about which would receive priority if a choice of one or the other had to be made.
One hospital representative’s response exemplified the lack of clarity and transparency during the calls by claiming, “If the situation is truly life-threatening, decisions will be made,” without explaining what qualifies as “life-threatening,” how those decisions would be made, or by whom.
Finally, miscarriage management procedures previously available to patients appeared to have been restricted in some hospitals after the passage of recent abortion laws in Oklahoma. For example, several hospitals cited the new “heartbeat law” (S.B. 1503) as the reason why they no longer perform procedures in cases of miscarriage. At seven hospitals, representatives avoided answering questions about cases in which the life of a patient with a viable pregnancy would be at risk. At one hospital, for example, the nurse repeatedly shifted the discussion to cases in which “there is no fetal heartbeat.” In those cases, the nurse stated, “When we have a situation where a baby no longer has a heartbeat, that’s between the physician and patient how to move forward.”
The study’s findings demonstrate that despite apparently good-faith efforts from most hospital representatives, callers could access little information, and the information they received was often conflicting and confusing – at some hospitals, callers received contradictory information from separate staff within the same hospital. These findings raise grave concerns about the ability of a pregnant person in Oklahoma – and other states with similar abortion bans – to receive clear, sufficient, and necessary information to make informed decisions about their medical care, and the ability of such patients to receive medically-necessary treatment. Callers also found that some hospital administrations, in an effort to comply with state laws, imposed restrictive policies on medical personnel that would impede their ability to provide prompt and effective care for pregnant patients.
At most hospitals, the callers were not provided reassurance that the pregnant patient’s life would be prioritized in medical decision-making.
1. Staff at Most Hospitals Provided No Information or Conflicting Information on Hospital Policies or Guidelines for Clinical Decision-Making in Medical Emergencies
At the start of every call, the callers asked hospital staff, “What are your hospital’s procedures if I were to face a medical emergency while pregnant that jeopardizes my life?” In response, staff at 22 hospitals (65 percent) were unable to provide information about procedures, policies, or support provided to doctors during medical emergencies when the clinical decision was that it was necessary to terminate a pregnancy to save the life of a pregnant patient. Staff at eight hospitals recommended that callers set up appointments with a doctor affiliated with the hospital, to ask them directly how they would approach medical emergencies and to discuss specific health concerns. In some cases, the callers were assured that through these appointments, they could learn more about each doctor’s views on these issues to help them select their preferred provider. However, when patients have an emergency, they are unlikely to be able to ensure that they receive care from a preferred provider.
Three hospitals stated that they were aware of internal policies but that they were not willing to share specific procedural information with the callers. Of these three:
- One hospital told the caller that she could not receive additional information about hospital guidelines for doctors until she was a patient at the hospital.
- Another hospital representative stated that guidelines are for internal use only and are not shared with patients.
- One representative offered to email the hospital’s written policies for handling emergency pregnancy situations, with the approval of her supervisor. However, although the caller left her email address with the staff member and contacted the hospital to confirm that they were sending the written policies, the information was never sent.
These findings raise grave concerns about the ability of a pregnant person in Oklahoma – and other states with similar abortion bans – to receive clear, sufficient, and necessary information to make informed decisions about their medical care, and the ability of such patients to receive medically-necessary treatment.
The callers were able to talk directly with nurses at six hospitals (approximately 18 percent). However, the information the clinicians provided was often no clearer than that provided by other hospital representatives. Although clinicians initially provided more information about the approval process required to terminate a pregnancy at their hospital (five of six nurses), compared to labor and delivery receptionists (13 of 28 receptionists), their seemingly greater knowledge about hospital policies was undercut by a tendency to provide incorrect information or to advise receptionists and other staff to withhold information from the callers. Some receptionists put callers on hold to consult with nurses or physicians and, upon their return, told the callers that they had been advised not to answer any questions about hospital policies. For instance:
- After consulting with a nurse, one hospital representative merely repeated in response to each of the caller’s questions, “I cannot advise on that.”
- At another hospital, a staff member who consulted with a physician returned to the call and reported (incorrectly) that “Nowhere in the state of Oklahoma can you get an abortion for any reason.”
In such cases, callers’ inability to access information could not be attributed to failure to reach medical experts; rather, clinicians did not provide accurate or meaningful information to the callers.
In two of the 11 hospitals in which callers spoke with multiple hospital representatives during a call, the callers received conflicting accounts of internal policies. At one hospital, two different staff members with whom the caller spoke provided contradictory information about the role of an ethics committee in decision-making during medical emergencies. Within the same call, one representative claimed that doctors would need the approval of an ethics committee to “sign off” on all determinations that a pregnancy needed to be terminated to save the life of the pregnant patient, whereas another stated that the committee is only required to sign off when patients are incapacitated and unable to communicate their preferences to a doctor.
Similarly, hospital staff conveyed a lack of knowledge and provided incorrect information about state laws affecting emergency pregnancy care in Oklahoma. For instance:
- Of the nine cases (27 percent) in which hospital representatives explicitly discussed the Oklahoma abortion bans, three explained that they did not know how recent laws would change the types of care hospitals can provide.
- One hospital representative asserted that ending a pregnancy as a treatment for a medical emergency “do[es] not count” as an abortion procedure under state law.
In calls with two hospitals, staff revealed that there were disagreements and discontent among medical professionals in their facilities about their hospitals’ responses to the new abortion bans. In one call, a nurse noted that there was a difference of opinion among physicians at their facility on how to act in emergency pregnancy situations, as well as on what constitutes an “emergency.” Similarly, a staff member at another hospital noted that not all nursing staff were “on board” with how their hospital had been providing care since the new state abortion laws.
At 10 hospitals, most of which were smaller and in non-urban areas, staff explained that patients would be transferred to another hospital if complications arose because their facility lacked the capacity to handle high-risk cases. But in none of those instances could the representative convey information on the policies of the facility to which they would be sending patients.
In sum, hospital representatives frequently demonstrated confusion, uncertainty, and lack of knowledge about the state of emergency obstetric care in the wake of Dobbs. No representatives were able or willing to share internal written policies with patients, even in cases where they indicated knowledge that their hospitals had such policies. And in those instances where clinicians were consulted, they often provided conflicting and incorrect information about hospital policies and state laws.
Hospital representatives frequently demonstrated confusion, uncertainty, and lack of knowledge about the state of emergency obstetric care in the wake of Dobbs.
It is important to note that at almost all the hospitals reached, staff responded to the callers in an empathetic manner and sought to reassure them about their commitment to patient safety and well-being. A staff member at one hospital reassured the caller of their extensive track record of handling similar cases, claiming that “we are the highest high-risk hospital in Oklahoma.”
Staff members at seven hospitals (21 percent) assured the callers that the safety of the pregnant patient is of paramount importance to medical personnel.
- At one hospital, a staff member emphasized that, “We want to take care of the mom and baby, but we’ll have to take care of you first.”
- In another case, the caller was reassured that, “You don’t need to be on the edge of dying before doctors act.”
- Some hospital staff explicitly expressed sympathy for the callers’ worries, explaining that they “completely understand” why callers were concerned following recent abortion bans and noting that their questions were “good questions to ask.”
Even at hospitals where staff sought to reassure the callers, however, they were not able to provide information on hospital policies that would back up their assurances. Indeed, one representative seemed to recognize the dual loyalty predicament clinicians now face in Oklahoma, stating that, “It is tricky because of state laws, but we will not let the mom die.”
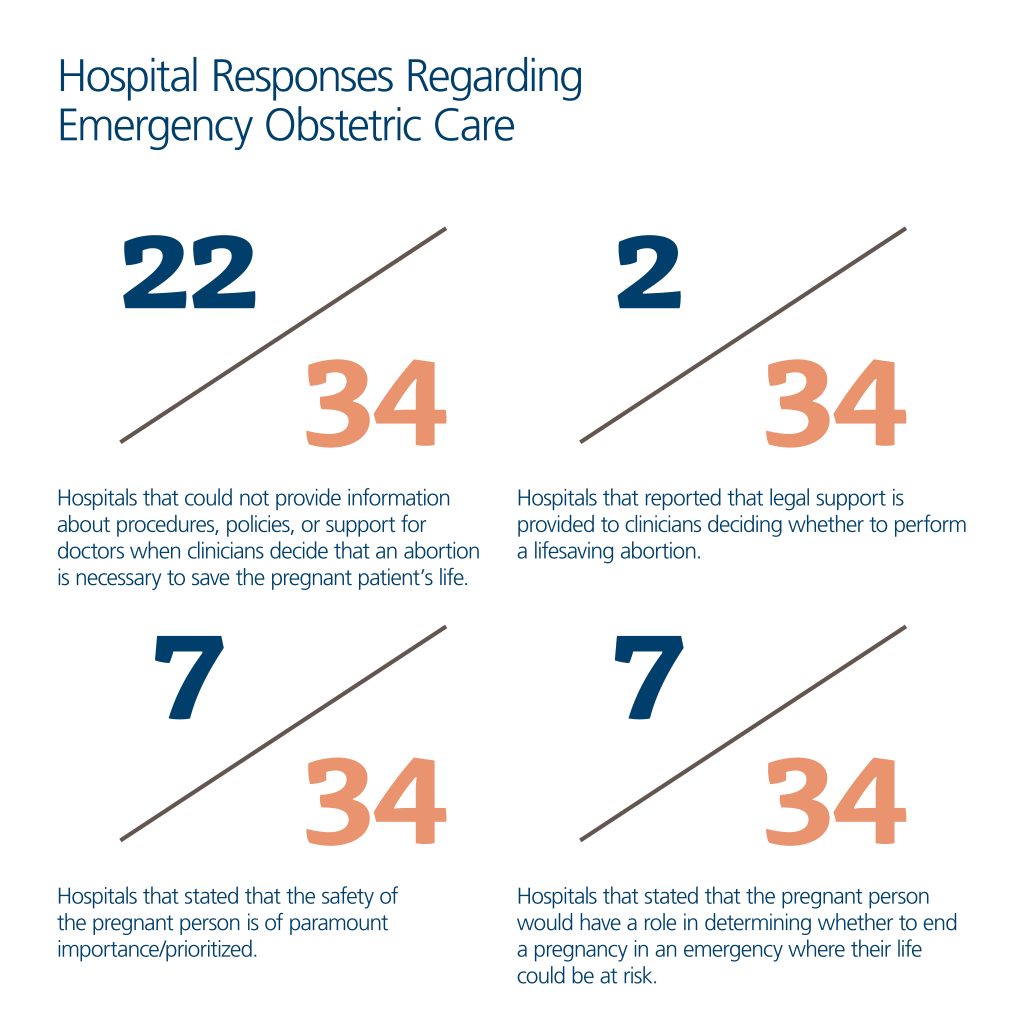
At one hospital, a staff member emphasized that, “We want to take care of the mom and baby, but we’ll have to take care of you first.” In another case, the caller was reassured that, “You don’t need to be on the edge of dying before doctors act.”
2. It Was Unclear What Criteria Clinicians Use in Determining When Pregnancies Can Be Legally Terminated
Few hospital representatives could provide clear answers to the callers about what criteria doctors might use to determine which medical conditions would classify as medical emergencies that threaten the pregnant person’s life, and, as a result, might warrant performing an abortion. While all patient care must be tailored to the condition and needs of the individual patient, individual clinicians may struggle to determine what level of danger to a patient’s health is legally required in order to permit an abortion, in addition to having differing views about medical necessity. As noted by one receptionist, “Not all doctors agree with each other on how emergency decisions are made and what emergency care should look like.” Representatives at seven hospitals (21 percent) shared examples of criteria that might be used to determine whether a life-threatening medical emergency exists. These included assessing the amount of vaginal bleeding (three hospitals), if the patient presents with a uterine infection or is septic (i.e., has a systemic, life-threatening infection) (two hospitals), or if they present with an ectopic pregnancy (two hospitals).
At one hospital, the representative both mischaracterized procedures to remove ectopic pregnancies as “abortions” and incorrectly described them as the only type of medical emergency that would meet Oklahoma’s legal criteria of saving the life of the pregnant person. She asserted that only ectopic pregnancies would count as medical emergencies that justify “abortion procedures,” drawing a false equivalence between ectopic pregnancies and other conditions that might warrant an abortion.[57]
The simulated patients also received little information about the guidance and support clinicians receive when deciding whether to terminate a pregnancy. Representatives at 16 hospitals (47 percent) suggested that doctors make decisions in such cases but did not provide any information about institutional guidance or support given to clinicians when they determine that a pregnancy should be terminated. Two hospital representatives noted that doctors receive legal counsel when they determine that a pregnancy needs to be terminated to save the life of the pregnant patient.
- In one instance, the caller was told that, in some cases, the hospital’s legal advisors and ethics board are consulted, but when they become involved “depends on the situation.”
- In the other instance, a hospital representative claimed that where the pregnant person’s life is possibly in danger and there is still a “fetal heartbeat,” medical staff would consult the legal team, but would still “not let the mother die.”
It is unclear from the information provided what role the legal counsel serves in these two hospitals. As a formal legal team defending against criminal or civil penalties, counsel could constitute a helpful support system for clinicians. However, internal policies that require legal counsel to sign off before physicians can terminate a pregnancy create procedural barriers that can delay necessary care and place pregnant patients at risk.
At three hospitals (nine percent), representatives stated that, although they would not perform “abortion procedures,” they would handle medical emergencies where the pregnant person’s life is in danger by inducing labor and delivering the fetus vaginally or with a cesarean section. Another three hospital representatives explained that they were uncertain about how new state laws would affect what procedures they can provide, and whether these would render previously acceptable procedures illegal.
3. In a Majority of Cases, Callers Received No Clear Information About Whether Internal Administrative Oversight Mechanisms Were Required to Provide Approval in Cases of Medical Emergencies
At four hospitals, representatives reported that a committee or another authority figure is required to sign off before the hospital can provide medically necessary abortions. These mechanisms include gaining approval from an ethics board (three hospitals) or a second doctor (one hospital). In one of these cases, the representative sought to reassure the caller that, although they required approval from an oversight committee, they would not let the patient die.
In another 14 cases (41 percent), hospital representatives provided unclear and/or incomplete answers about whether doctors require approval to perform a medically necessary abortion. One representative, for example, claimed that doctors at that hospital are not allowed to perform certain procedures for “ethical reasons,” but would not clarify what those procedures or ethical concerns are. It was unclear whether this representative meant that doctors require the approval of an internal ethics board, or that doctors should follow ethical guidelines created by national medical bodies such as the American College of Obstetricians and Gynecologists (ACOG). Many of these representatives also did not directly answer whether doctors were required to receive hospital approval to perform abortions, leaving the callers uncertain about hospital policy. In one case, the representative avoided answering the question by only discussing circumstances where the “fetus has no heartbeat.”

4. Hospital Staff Rarely Talked About Prioritizing Patient Safety, Patients’ Role in Making Decisions in Medical Emergencies, or Professional Ethics
The callers received little clarity about how patient input and safety would be prioritized during medical or obstetric emergencies. Staff members at 27 hospitals (79 percent) either did not offer information about patients’ roles in decision-making or, in one case, stated that, “You get a voice, but doctors make the final decision.” In two cases, patients were told that medical decisions “also depend on what your husband and family want.”
Hospital representatives at only seven hospitals (21 percent) affirmed to the callers that they would have a role in deciding whether to terminate a pregnancy in obstetric emergencies when their life could be at risk. For example:
- A staff member at one hospital stated, “It is entirely your decision how the doctors take care of you,” adding that they require the patient’s consent before performing any care.
- A representative at another hospital stated that patients can request a second opinion or involve the ethics review board if they disagree with the decision reached by their doctor about terminating a pregnancy in medical emergencies.
In the same vein, the callers received inconsistent and varied messaging about doctors’ priorities when treating medical emergencies in pregnant patients.
- Representatives at only seven hospitals (20 percent) voluntarily shared that their hospitals prioritize the life of the pregnant person. In two cases, hospital representatives explained that “We want to take care of the mom and baby but we’ll have to take care of you first,” and that the hospital staff would do “anything necessary to save [your] life because that is the [hospital name]’s way.”
- At six hospitals (18 percent), hospital representatives stated that, at their facility, the life of the pregnant person and fetus are prioritized equally.
- At one hospital, representatives suggested that during an emergency, medical personnel would use the pregnant person’s body as an “incubator” to carry the baby as long as possible.
Representatives at 21 hospitals (62 percent) offered no information on how staff prioritize saving the fetus over saving the life of the pregnant person in medical emergencies.
Finally, it was unclear to the callers whether hospital staff were aware of or actively considering how medical ethics and professional responsibilities affect the type of care provided to pregnant patients. Only two hospital representatives, for instance, noted that doctors follow the guidance of national medical associations such as ACOG.[58] Instead, most representatives never mentioned ACOG guidelines or any other relevant obligations, nor could they clearly define, when asked, the guidance that informed medical decision-making relating to abortion. One discussion about ethics and hospital responsibilities focused on the hospitals’ religious affiliation. In this case, hospital staff explained that their Catholic background meant that the administration already had rules similar to those in the recent abortion bans.
Representatives at only seven hospitals (20 percent) voluntarily shared that their hospitals prioritize the life of the pregnant person. At one hospital, representatives suggested that during an emergency, medical personnel would use the pregnant person’s body as an “incubator” to carry the baby as long as possible.
5. There Was Significant Variability among Hospitals about How Miscarriages Would Reportedly Be Handled, Especially Where There Was Still Fetal Cardiac Activity
When asked about the types of miscarriage management services offered, representatives at most of the hospitals reported that physicians were able to perform a wide range of treatment procedures in cases where there was no fetal cardiac activity. In the words of one nurse, “When we have a situation where a baby no longer has a heartbeat, that’s between the physician and patient how to move forward.” Representatives at 25 hospitals (74 percent) stated that dilation and curettage (D&C) and dilation and evacuation (D&E) – both techniques to remove fetal, placental, or uterine tissue after an incomplete or threatened miscarriage or as part of an abortion – are allowed at their hospitals when there is no detected fetal cardiac activity. Representatives at two hospitals avoided commenting on using D&C procedures to remove fetal tissue by only discussing placental tissue. The representative at one hospital stated categorically that their hospital prohibits D&E and D&C procedures after 16 weeks of pregnancy, even though many miscarriages occur after that point.
However, in situations where medical personnel detect fetal cardiac activity, few representatives were able to state that their hospital provides miscarriage management services necessary to protect the life of a patient. Five hospitals (15 percent) explained that, because of the “heartbeat law” passed in the state, doctors are not allowed to end a pregnancy when fetal activity is detected, regardless of the viability of the fetus. Seventeen hospitals (50 percent) explicitly told patients that D&C and D&E procedures are allowed during obstetric emergencies if there is detected activity, a third fewer than those who reported allowing these procedures in cases of no detected fetal cardiac activity. Geographically, the hospitals willing to perform D&C and D&E procedures in cases of fetal cardiac activity were primarily clustered in urban centers in the northern and central regions of Oklahoma. Of the 17 hospitals that allow D&C and D&E procedures in cases of fetal cardiac activity, two also imposed additional requirements: one obligated doctors to receive approval from a legal counsel, and the other stated that doctors must “exhaust other options” before performing the procedure.
These findings demonstrate the pernicious impact of Oklahoma’s laws on pregnant patients who are seeking to understand policies and procedures that might guide medical decision-making should they experience a medical emergency. They suggest that pregnant people in Oklahoma, and likely those in the other 12 states with similar laws, face significant obstacles and may be unable to receive necessary information to guide their decisions on where to receive obstetric care. The high frequency of inconsistent, incomplete, and unclear information the simulated callers received is alarming and suggests that hospitals in Oklahoma are struggling to articulate their response to obstetric emergencies in light of the state’s new abortion laws. Taken together, the study’s findings raise serious concerns about the impact of Oklahoma’s anti-abortion laws on patients’ right to information concerning their sexual and reproductive health and their right to receive appropriate, evidence-based care.
The study’s findings raise serious concerns about the impact of Oklahoma’s anti-abortion laws on patients’ right to information concerning their sexual and reproductive health and their right to receive appropriate, evidence-based care.
Legal and Ethical Standards
This case study focuses on the challenges that pregnant people face in getting information on how abortion bans in Oklahoma will affect their ability to receive life-saving care in the case of medical emergencies. That question further unfolds in a context in which hospitals themselves are struggling to navigate these laws, share clear information with prospective patients, and continue providing care that conforms with medical ethics. The inability of the hospitals called in this study to provide clear and accurate information about the care pregnant patients would receive if facing a pregnancy-related medical emergency at any given institution is a reflection of the untenable situation hospitals face under the current abortion bans.
The section below outlines how Oklahoma’s laws – and others like it – conflict with and depart from international human rights law and from the ethical guidelines issued by a range of professional medical associations.
Obligations under International Human Rights Law
International human rights law protects people’s access to reproductive health care and the exercise of reproductive decision-making.[59] Over the past 25 years, the international community has clarified that abortion is a fundamental human right, and jurisprudence from international human rights bodies establishes that access to abortion is necessary to protect the rights to health, life, non-discrimination, information, privacy, and freedom from ill-treatment, harmful practices, and gender-based violence.[60] In March 2022, the World Health Organization (WHO), the leading global public health expert body, published an updated Abortion Care Guideline, which recognizes abortion as an essential health service that is necessary for the realization of human rights.[61]
International human rights law protects people’s access to reproductive health care and the exercise of reproductive decision-making. Over the past 25 years, the international community has clarified that abortion is a fundamental human right.
Abortion access is essential to the right to health, which includes the right to reproductive and sexual health.[62] Accordingly, United Nations (UN) human rights treaty monitoring bodies have established that abortion, like other reproductive health care, must be available, accessible (including affordable), acceptable, and of good quality.[63] States (referring to government at all levels) must provide abortion services and information to all people who may require them.[64] In addition, pursuant to the right to health, states must address the underlying social determinants of health, which are comprised of the social, economic, and cultural factors that can determine an individual’s health.[65]
Abortion access is also critical to the right to life. UN human rights bodies have long recognized and reinforced the WHO’s findings that restrictive abortion laws lead to high rates of unsafe abortions and attendant maternal mortality and morbidity.[66] And they have repeatedly ruled that states should protect people from the physical and mental health risks associated with unsafe abortions.[67] Consistent with this recognition, the UN Human Rights Committee, which is charged with overseeing interpretation and implementation of the International Covenant on Civil and Political Rights, a treaty ratified by the United States, has confirmed that the right to life contains important protections for access to abortion. It limits the restrictions that states can place on abortion access and obligates governments to ensure access to abortion, at a minimum where a person’s life and health are at risk, or when carrying a pregnancy to term would cause substantial pain or suffering.[68] Other treaty bodies have likewise found that access to safe and legal abortion is essential to reproductive health and a prerequisite to safeguarding the right to life, among other rights.[69]
Accurate information about abortion care is likewise critical to ensuring that people can exercise their reproductive rights.[70] The UN Special Rapporteur on the right to health has confirmed that criminalization of sexual and reproductive health services generates “a chilling effect on the open exchange of information,” and “[w]here narrow exceptions to the criminalization of abortion exist, such as to save the life of a woman, criminalization may effectively block access to information about legal abortion services.”[71] States have an obligation to provide access to comprehensive, accurate, and evidence-based information on abortion services, including on the legality of abortion and how to access safe abortion services and post-abortion care.[72] The right to information requires states to make this information accessible to all individuals, including adolescents and youth, without needing the consent of legal guardians.[73] States must ensure that health care providers give medically accurate and non-stigmatizing information on abortion, while also guaranteeing patient confidentiality.[74] And states also must ensure that information is accessible, and that people can seek, receive, and disseminate evidence-based, medically accurate, and unbiased information regarding abortion, as well as receive specific information on their individual health status.[75]
States have an obligation to provide access to comprehensive, accurate, and evidence-based information on abortion services, including on the legality of abortion and how to access safe abortion services and post-abortion care.
Consistent with these and other human rights protections (including the rights to equality and non-discrimination, privacy, and freedom from torture or cruel, inhuman, or degrading treatment), UN human rights treaty bodies have condemned the criminalization of abortion and expressed concern about the impact of severe legal restrictions and barriers on abortion access, as well as expressed concern about abortion stigma.[76] UN treaty bodies have urged states to provide financial support for those who cannot afford abortion services.[77] And the Human Rights Committee has recognized that national laws prohibiting abortion – thereby forcing people to choose between continuing a pregnancy and traveling to another country to access legal abortion services (for those able to travel) – can cause anguish and suffering, including financial, social, and health-related burdens and hardships.[78]
UN human rights law has increasingly recognized the state obligation to ensure that access to abortion includes full decriminalization.[79] UN treaty bodies and experts’ recommendations no longer only call for reform where states criminalize abortion without exceptions or in limited circumstances. Rather, such recommendations now explicitly urge full decriminalization, as well as positive measures to guarantee access to abortion, “at least” on specific grounds such as risk to life or health, for victims of rape and incest, and due to the existence of severe or fatal fetal impairment.[80]
U.S. regression on abortion rights, as exemplified by the abortion bans in Oklahoma, has been widely condemned as a violation of human rights. Responding to the U.S. Supreme Court’s decision in Dobbs v. Jackson Women’s Health Organization, then-UN High Commissioner for Human Rights Michelle Bachelet reiterated human rights protections for those seeking or providing abortions and the impact that the decision will have on the fundamental rights of millions within the United States, particularly people with low incomes and people belonging to racial and ethnic minorities.[81] UN independent human rights experts, including the UN Working Group on discrimination against women and girls, the UN Special Rapporteur on health, and the UN Special Rapporteur on violence against women, similarly denounced the decision in Dobbs.[82] At the conclusion of a human rights review of the United States in August 2022, the UN Committee on the Elimination of Racial Discrimination noted deep concerns with the Dobbs decision and recommended that the United States address the disparate impact that it will have on racial and ethnic minorities, Indigenous women, and those with low incomes.[83]
Medical Ethics Obligations of Health Care Professionals
In the United States, the professional membership organizations for professionals involved in reproductive and pregnancy-related health care are unambiguous in their opposition to laws that restrict their patients’ access to abortion services as part of their health care and that erect barriers to their members’ ability to practice evidence-based medicine. Professional organizations representing obstetrician-gynecologists, family physicians, and midwives, among the specialties involved in reproductive, prenatal, and peri- and postpartum care in the United States, are united in their reasons for opposing abortion laws like those in Oklahoma. Professional associations have denounced the threat of criminal liability under recent abortion bans for their potential chilling effect on the provision of evidence-based medical care in line with ethical obligations. For example, the American College of Obstetricians and Gynecologists (ACOG) has noted:
In states with laws criminalizing abortion provision, clinicians may be nervous to provide pregnant patients with needed diagnostic tests (i.e., radiology imaging) or interventions (i.e., anesthesia or surgical intervention for a ruptured appendix during pregnancy) due to fear of inadvertently causing a pregnancy loss. They may also be confused about the impact of abortion restrictions on miscarriage and pregnancy of unknown location management. In addition, they may be uncertain about what they should document in the medical record when caring for particular patients.[84]
ACOG has underscored the important role of hospitals in states with abortion bans in helping providers who seek to uphold medical standards of care and ethics:
It is important that clinicians feel supported by their hospitals to provide and connect pregnant patients with necessary care. This may involve setting up meetings between clinicians and the hospital’s legal counsel to review risks and discuss how the hospital will support and protect clinicians. It may also involve establishing hospital policies emphasizing clinicians’ responsibility to provide compassionate, evidence-based, and non-judgmental care to their patients in whatever way they can. Institutions can also bring in trainers to help clinicians understand best practices for preventing criminalization of pregnant patients who may present, for example, after self-managing an abortion.[85]
While these measures can help provide some support to clinicians navigating the legal and professional risks arising from these laws, ultimately, medical associations have affirmed the unworkability of these laws. ACOG has reaffirmed that “[d]octors and other health care professionals must be able to assess the unique patient and clinical situation in front of them and make reasonable, evidence-based decisions about when to intervene without fear of prosecution, loss of license, or fines.”[86]
“Doctors and other health care professionals must be able to assess the unique patient and clinical situation in front of them and make reasonable, evidence-based decisions about when to intervene without fear of prosecution, loss of license, or fines.”
American College of Obstetricians and Gynecologists
ACOG has unequivocally opposed “any effort that impedes access to abortion care and interferes in the relationship between a person and their health care professional. Because the patient-clinician relationship is a critical component of the provision of the highest quality health care, any efforts interfering in this relationship harm the people seeking essential health care and those providing it.”[87] It has specifically criticized state legislators “taking it upon themselves to define complex medical concepts without reference to medical evidence” and passing “vague, unscientific laws.” ACOG forcefully disagrees with the premise that “[e]lected politicians, who lack our members’ education, training, experience, expertise, and responsibility to patients, can or should be in the exam room weighing those factors or in a position of substituted judgment for our members and their patients.”[88]
ACOG’s position is echoed by the American Academy of Family Physicians (AAFP), the American College of Nurse-Midwives (ACNM), and the American Medical Association (AMA), among others.
In response to the Dobbs ruling, the AAFP, ACOG, the AMA, and 75 other health care organizations released a statement unequivocally opposing legislative interference in the patient-physician relationship. Like ACOG, the AAFP states that it “supports access to comprehensive pregnancy and reproductive services, including but not limited to abortion, pregnancy termination, contraception, and surgical and non-surgical management of ectopic pregnancy, and opposes nonevidence-based restrictions on medical care and the provision of such services.”[89] Similarly, the AAFP opposes legislation that infringes on the content or breadth of information exchanged within the patient-physician relationship and legislation that interferes with the provision of evidence-based medical care, either of which “can harm the health of the patient, the family, and the community.”[90]
The ACNM has joined with ACOG and AAFP in condemning laws restricting their patients’ access to abortion services as a necessary part of the “full-range of preventive, reproductive, and sexual health services.”[91] The ACNM affirms that “everyone has the right to decide what is best for their health, bodies, lives, and families. As such, we adamantly oppose all legal opinions and legislative policy that blatantly or surreptitiously seek to restrict or ban the provision of abortion care, as well as any efforts at any level to render it less accessible.”[92]
In response to new state laws such as those in Oklahoma, professional organizations are publishing new guidance for clinicians on how to navigate their dual loyalty constraints. The AMA, the largest membership organization of physicians across all specialties in the United States, revised its Principles of Medical Ethics in November 2022 to clarify that physicians are permitted to perform abortions as part of good medical practice. In their press release on the revised principles, the AMA noted that:
This is in alignment with the AMA’s opposition to government intrusion into the therapeutic alliance between patients and physicians, as such intrusion prevents physicians from exercising their professional judgment and undermines their obligation to protect the well-being of their patients.[93]
The AMA clarified its principles to recognize that where the “letter of the law would foreclose urgently needed care, physicians must have latitude to act in accord with their best professional judgment,” including explicitly in the context of abortion.[94]
The AMA has committed to providing support, including legal support, to physicians and medical students where needed and additional resources to help physicians navigate the ethical and legal aspects of the post-Dobbs era. AMA statements affirm the association’s commitment to oppose criminal charges against patients or physicians when pregnancy loss results from medically necessary treatment for cancer and other illnesses. The AMA also will advocate that physicians and patients should not be held civilly or criminally liable in cases when pregnancy loss results from medically necessary care. As Dr. Resneck succinctly described, “Under extraordinary circumstances, the ethical guidelines of the profession support physician conduct that sides with their patient’s safety and health, acknowledging that this may conflict with legal constraints that limit access to abortion or reproductive care.”[95]
Federal and State Legal Obligations
In support of these ethical guidelines, the federal government has clarified through Health and Human Services (HHS) guidance that the Emergency Medical Treatment and Active Labor Act (EMTALA) obligates physicians to provide stabilizing care, including abortion where medically appropriate, when a patient presenting at an emergency department is experiencing an emergency medical condition. While EMTALA indicates that abortion may be considered stabilizing care where needed to ensure that a patient will not have their health placed in serious jeopardy, have their bodily functions seriously impaired, or suffer serious dysfunction of any bodily organ or part, state laws are often more restrictive. State laws, as is the case in Oklahoma, may require that the individual’s life already be in danger prior to an abortion being permitted. HHS’s EMTALA guidance has been challenged by states with near abortion bans as being preempted by state law, with differing outcomes in different states.
The current legal framework in Oklahoma impedes hospitals and clinicians from fulfilling their ethical and professional responsibilities.
At the state level, Oklahoma law imposes stringent requirements for informed consent that are inconsistent with the hospitals’ inability to share information about what care patients may receive in certain circumstances.[96] Under Oklahoma Supreme Court precedent, a physician “should disclose all courses of treatment that are medically reasonable under the circumstances” and “is not permitted to withhold any facts which are necessary to form an intelligent consent by the patient to the proposed treatment.”[97] S.B. 1503, however, chills clinicians from sharing information with patients about abortion procedures by creating civil liabilities for anyone who “knowingly engages in conduct that aids or abets the performance or inducement of an abortion.”[98]
On September 21, 2022, the Oklahoma State Medical Association, ACOG, AMA, and the Society for Maternal-Fetal Medicine all signed an amicus curiae brief to the Oklahoma Supreme Court calling for an injunction of state abortion bans because they deprive individuals of their “inherent right to life [and] liberty,” particularly the right to bodily autonomy and integrity in making decisions about health care.[99] According to these organizations, “laws that criminalize and effectively ban abortion deprive pregnant patients of their rights to access a safe and essential component of reproductive health care without any medical or scientific justification.”[100]
Similarly, the American Bar Association “opposes governmental actions and policies that interfere with patients’ abilities to receive from their health care providers, including health care professionals and entities, in a timely manner: (a) all of the relevant and medically accurate information necessary for fully informed health care decision-making; and (b) information with respect to their access to medically appropriate care, as defined by the applicable medical standard of care, whether or not the provider chooses to offer such care.”[101]
In practice, the dual loyalties that clinicians face in states like Oklahoma are clear. Delaying access to abortion procedures until the patient is in a critical condition can result in the death of the patient or serious morbidities. On the other hand, providing a medically beneficial abortion before this point could result in criminal and financial penalties. The current legal framework in Oklahoma impedes hospitals and clinicians from fulfilling their ethical and professional responsibilities.
Conclusion and Recommendations
These findings affirm what has been recognized by the World Health Organization: that the criminalization and penalization of abortion care – even with an exception for medical necessity – is fundamentally inconsistent with evidence-based, ethical, and patient-centered health care, and with human rights.
Based on the findings of this report, not a single hospital in Oklahoma appeared to be able to articulate clear, consistent policies for emergency obstetric care that supported their clinicians’ ability to make decisions based solely on their clinical judgement or clearly explain how a prospective patient’s life would be prioritized or protected if faced with an obstetrical emergency. Oklahoma’s multiple, overlapping, and punitive abortion laws cause confusion regarding clinicians’ ability to provide health and life-saving care during obstetric emergencies without punishment.
These findings also underscore how health care providers in Oklahoma are placed in a situation of dual loyalty, forcing them to balance their obligation to provide ethical, high-quality medical care against the threat of legal and professional sanctions. Health professionals are effectively prevented from providing patient-centered care consistent with established medical and ethical standards of care, while pregnant people seeking obstetric care in the state are unable to obtain the information necessary to make informed decisions about their own health care. These risks are further compounded for populations already facing significant challenges and barriers in accessing essential medical care, including bias and discrimination.
Oklahoma’s abortion bans raise serious human rights concerns, including relating to violations of individuals’ rights to life, health, equality, information, freedom from torture and ill-treatment, and freedom to exercise reproductive autonomy. These findings affirm what has been recognized by the World Health Organization: that the criminalization and penalization of abortion care – even with an exception for medical necessity – is fundamentally inconsistent with evidence-based, ethical, and patient-centered health care, and with human rights.
Because the current legal status is untenable, Physicians for Human Rights, Oklahoma Call for Reproductive Justice, and the Center for Reproductive Rights make the following recommendations:
To the Oklahoma Legislature:
- Repeal Oklahoma’s abortion bans and decriminalize abortion. Remove all civil and legal penalties for abortion, including against health care providers.
- Ensure that health care services for pregnant people and all Oklahomans are accessible and of good quality. Policies should facilitate and expand, not limit, access to health care for people in Oklahoma. They should also address Oklahoma’s maternal mortality disparities and disparities in underlying social determinants of health that cause certain communities, including Black, Indigenous, and other Oklahomans of color, to experience adverse health outcomes.
To Oklahoma’s Hospitals and Health Care Professionals:
- Speak out against laws criminalizing abortion or otherwise restricting access to abortions, including during obstetric emergencies. Health care professionals and institutions should speak out about how abortion bans harm patients, undermine the ability of health care providers to fulfill their professional and ethical obligations, and are inconsistent with evidence-based, patient-centered, and ethical medical care.
- Build knowledge and awareness of professional recommendations and guidance for providing abortion services. Oklahoma hospitals and other health care providers must better ensure that staff and clinicians in clinical settings are acting in accordance with the recommendations that the American Medical Association (AMA), the American College of Obstetricians and Gynecologists (ACOG), and other medical professional organizations have made affirming ethical and professional obligations to provide abortion services to patients.
To State and National Medical Associations:
- Publicly condemn abortion bans and continue to speak out against the dual loyalty impacts of abortion bans, including citing evidence of how such laws undermine ethical obligations and professional duties of care. Associations such as the AMA and ACOG, including their state chapters, should advocate against this undue interference in the practice of medicine and engage at the state and national level to remove civil and legal penalties for abortion and maternal health care, and to secure rights.
To the Federal Government:
- Enact and implement national laws and policies that ensure rights and remove barriers to abortion care and maternal health care. Ensure that all people can access comprehensive reproductive health care with dignity, free from discrimination and criminalization, regardless of where they live.
To Professionals Who Provide Social, Legal, and Related Services to Pregnant People in Oklahoma and Nationally:
- Support pregnant people in navigating barriers to access the care they need. Social workers, mental health counselors, domestic violence assistance organizations, legal services providers, and other professionals should advocate for their clients to receive medically appropriate care, including abortions when necessary to preserve their health or life.
- Raise awareness of the discriminatory impacts and harms of laws criminalizing abortion. Professionals who provide support services to pregnant people are uniquely positioned to understand and speak out against the practical impact of abortion bans on their clients, including pregnant people for whom abortion may be necessary to preserve their health or life.
To Social Justice Advocates in Oklahoma and Nationally:
- Adopt an intersectional approach supporting solidarity in opposing abortion bans and supporting reproductive autonomy. Advocates for racial and economic justice, for bodily autonomy, for patients and providers, and for families and children should join reproductive health, rights, and justice advocates in opposing abortion bans and supporting pregnant people’s ability to access reproductive health care.
To Researchers and Research Institutes:
- Continue to systematically monitor and evaluate the impact of abortion bans on patients and providers. Build on existing research and share information to deepen awareness and understanding of the full scope of harms resulting from restrictive abortion laws and the criminalization of abortion services.
Acknowledgements
This report is a joint product of Physicians for Human Rights (PHR), the Oklahoma Call for Reproductive Justice (OCRJ), and the Center for Reproductive Rights (CRR).
The report was researched and written by PHR staff members Christian De Vos, JD, PhD, director of research and investigations; Michele Heisler, MD, MPA, medical director; William Jaffe, Aizik Wolf Fellow; and Payal Shah, JD, director of the Program on Sexual Violence in Conflict Zones; Tamya Cox-Touré, JD, OCRJ chair; and Priya Desai, MSW, OCRJ board member; and CRR staff members Nimra J. Chowdhry, JD, senior state legislative counsel; Risa Kaufman, JD, director, U.S. Human Rights; and Rabia Muqaddam, JD, senior staff attorney.
The report was reviewed by PHR staff members Erika Dailey, MA, director of advocacy and policy; Karen Naimer, MA, JD, LLM, director of programs; Ranit Mishori, MD, MHS, senior medical advisor; Michael Payne, deputy director, advocacy; Kevin Short, deputy director, media and communications; and Saman Zia-Zarifi, JD, LLM, executive director; and by Sandy Keenan, CRR’s senior director, marketing and communications. CRR staff members Tamar Eisen, program coordinator, Judicial Strategy; Lauren Elfant, JD, deputy director U.S. Program; Pilar Herrero, JD, senior human rights counsel; and Lourdes Rivera, JD, senior vice president U.S. Program Emerita also supported the project.
Calls to hospitals in Oklahoma were conducted by PHR graduate school interns Caytlin Schultz and Rachael Burton. Samantha Peck, PHR program and executive associate, also called hospitals and contributed to the writing of the report, as well as providing overall project support.
The report benefitted from external review by Angela Hawkins, MD, an obstetrics and gynecology specialist, and Susan M. Blaustein, MMA, DMA, PHR board member and founder/director of WomenStrong.
The report was reviewed, edited, and prepared for publication by Claudia Rader, MS, PHR’s senior publications consultant.
PHR, OCRJ, and CRR are grateful for the efforts of staff at the Oklahoma hospitals that were contacted, who took time to answer callers’ questions.
Endnotes
[1] Press release, Department of Justice, Garland Statement on Supreme Court Ruling in Dobbs v. Jackson Women’s Health Organization (Jun. 24, 2022), https://www.justice.gov/opa/pr/attorney-general-merrick-b-garland-statement-supreme-court-ruling-dobbs-v-jackson-women-s.
[2] “Heartbeat” is an inaccurate term referring to the rudimentary electrical activity that occurs around five or six weeks in an embryo or fetus. The embryo or fetus at that stage has not developed a “heart.” See also 63 Okla. Stat. §§ 1-745.34-45; 21 Okla. Stat. § 861; 63 Okla. Stat. §§ 1-731.4.
[3] As used in this report, the term “abortion bans” refer to prohibitions of abortion after conception. Restrictions on abortion after a certain number of weeks (“gestational limits”) are not included in this term. There are additional states beyond the 13 identified where laws banning abortions have been written but are not in effect, due to court injunctions or opposition by state governors and attorneys general. See also, After Roe Fell: Abortion Laws by State, Center for Reproductive Rights (CRR), https://reproductiverights.org/maps/abortion-laws-by-state/.
[4] Ark. Code Ann. § 5-61-301 to –304; See, e.g., After Roe Fell: Arkansas, CRR, https://reproductiverights.org/maps/state/arkansas/.
[5] Miss. Code Ann. § 41-41-45; See, e.g., After Roe Fell: Mississippi, CRR, https://reproductiverights.org/maps/state/mississippi/.
[6] S.D. Codified Laws § 22-17-5.1; See, e.g., After Roe Fell: South Dakota, CRR, https://reproductiverights.org/maps/state/south-dakota/.
[7] Alyssa Llamas et al., Jacobs Inst. of Women’s Health, Geo. Wash. Univ. & the Clara Schiffer Project on Women’s Health, Public Health Impacts of State-level Abortion Restrictions Overview of Research & Policy in the United States 1, (Apr. 2018), https://publichealth.gwu.edu/sites/default/files/downloads/projects/JIWH/Impacts_of_State_Abortion_Restrictions.pdf; Erin Durkin, ‘Women Will die’: How New Abortion Bans Will Harm the Most Vulnerable, The Guardian (May 19, 2019), https://www.theguardian.com/us-news/2019/may/19/abortion-ban-alabama-women-of-color-poor; Liza Fuentes, Latina Immigrant Women’s Access to Abortion: Insights from Interviews with Latina Grasstops Leaders, Nat’l Latina Inst. for Reprod. Health 1-4 (Sep. 2010), https://nciwr.files.wordpress.com/2011/01/nlirh-reserach-brief-sept2010-final1.pdf; National Council on Disability, The Current State of Health Care for People with Disabilities 51–52, 54–56, (2009), https://ncd.gov/publications/2009/Sept302009#Health%20Status; Megan K. Donovan, In Real Life: Federal Restrictions on Abortion Coverage and the Women They Impact, Guttmacher Inst. (Jan. 5, 2017), https://www.guttmacher.org/gpr/2017/01/real-life-federal-restrictions-abortion-coverage-and-women-they-impact.
[8] These states are Arkansas, Oklahoma, South Dakota, and Texas, see State Bans on Abortion Throughout Pregnancy, Guttmacher Inst. (Feb. 1, 2023), https://www.guttmacher.org/state-policy/explore/state-policies-later-abortions.
[9] Alabama, Kentucky, Missouri, and Tennessee have exceptions for only life and health (“severe permanent damage to major organs or bodily functions”). Louisiana and West Virginia currently have exemptions for a list of fetal anomalies in addition to life and health. Idaho and West Virginia have rape exceptions in addition to life and health, Mississippi has a rape exception in addition to life, and Idaho and West Virginia also have incest exceptions in addition to life and health, see ibid.
[10] In the face of concerns about the vagueness of exceptions, several lawmakers have attempted to create lists of specific conditions or criteria under which abortion is legally permitted. However, this approach fails for several reasons. First, pregnancy is a complex condition, and it is impossible to contemplate every circumstance that may come up where a termination may be clinically indicated. See, e.g., Understanding and Navigating Medical Emergency Exceptions in Abortion Bans and Restrictions, Am. Coll. of Obstetricians and Gynecologists (ACOG) (Aug. 15, 2022), https://www.acog.org/news/news-articles/2022/08/understanding-medical-emergency-exceptions-in-abortion-bans-restrictions (outlining why lists of conditions that qualify as “medical emergencies” are impossible to create and are unworkable). Second, even where there is a list of criteria or conditions, there may still be confusion around the certainty or severity of the diagnosis. See, e.g. World Health Org., Abortion Care Guideline, 21-30 (2022), https://www.who.int/publications/i/item/9789240039483. Third, it is clear from international human rights jurisprudence that even where countries have broad exceptions, the continued criminalization of abortion continues to hinder abortion access by creating stigma and fear amongst health care providers. See, e.g., Comm. on the Elimination of Discrimination against Women (CEDAW), Inquiry Concerning the United Kingdom of Great Britain and Northern Ireland under article 8 of the Optional Protocol to the Convention on the Elimination of All Forms of Discrimination against Women, ¶¶17-20, U.N. Doc. CEDAW/C/OP.8/GBR/1 (Mar. 6, 2018); CEDAW, Concluding Observations on the Sixth Periodic Report of Nepal, ¶¶ 38-39, UN Doc. CEDAW/C/NPL/CO/6 (Nov. 14, 2018).
[11] See Physicians for Human Rts. & the Sch. of Pub. Health and Primary Health Care Univ. of Cape Town, Dual Loyalty & Human Rights In Health Professional Practice: Proposed Guidelines & Institutional Mechanisms, 11-13 (2002), https://phr.org/wp-content/uploads/2003/03/dualloyalties-2002-report.pdf.
[12] Press Release, AMA announces new adopted policies related to reproductive health care, AMA, (Nov. 16, 2022), https://www.ama-assn.org/press-center/press-releases/ama-announces-new-adopted-policies-related-reproductive-health-care.
[13] Anita Wadhwani, “In open Letter, 700 Tennessee healthcare providers call on Legislature to ‘reconsider’ abortion ban,” Tennessee Lookout(Oct. 10, 2022), https://tennesseelookout.com/briefs/in-open-letter-700-tennessee-healthcare-providers-call-on-legislature-to-reconsider-abortion-ban/.
[14] Piper Hutchinson, “Doctors spell out their opposition to Louisiana’s abortion law,” Louisiana Illuminator (Jul. 6, 2022), https://lailluminator.com/2022/07/06/doctors-spell-out-their-opposition-to-louisianas-abortion-law/.
[15] See Prelabor Rupture of Membranes, ACOG (Mar. 2020), https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2020/03/prelabor-rupture-of-membranes; See also, What are some common complications of pregnancy?, NICHD Eunice Kennedy Shriver Nat’l Inst. of Child Health and Hum. Dev., https://www.nichd.nih.gov/health/topics/pregnancy/conditioninfo/complications.
[16] Carla Dugas & Valori H. Slane, Miscarriage, (Jun. 27, 2022), https://www.ncbi.nlm.nih.gov/books/NBK532992/.
[17] Rosemary Westwood, “Bleeding and in pain, she couldn’t get 2 Louisiana ERs to answer: Is it a miscarriage?,” NPR (Dec. 29, 2022), https://www.npr.org/sections/health-shots/2022/12/29/1143823727/bleeding-and-in-pain-she-couldnt-get-2-louisiana-ers-to-answer-is-it-a-miscarria.
[18] As noted above, “heartbeat” is an inaccurate term referring to the rudimentary electrical activity that occurs around five or six weeks in an embryo or fetus. Six-week gestational limits use the term “fetal heartbeat,” although the embryo or fetus at that stage has not developed a “heart.”
[19] Mikhaila Richards, The Public, Including Women of Childbearing Age, Are Largely Confused About the Legality of Medication Abortion and Emergency Contraceptives in Their States, Kaiser Family Foundation (Feb. 1, 2023), https://www.kff.org/womens-health-policy/press-release/the-public-including-women-of-childbearing-age-are-largely-confused-about-the-legality-of-medication-abortion-and-emergency-contraceptives-in-their-states/.
[20] Nicole Einbinder and Caroline Haskins, “Oklahoma lawmakers passed 5 contradictory abortion bans. No one knows which laws will be enforced,” Business Insider (Jun. 24, 2022), https://www.businessinsider.com/oklahoma-abortion-ban-sponsors-dont-know-what-law-might-be-post-roe-2022-5?op=1.
[21] See Memorandum from Okla. Att’y Gen. to All Okla. Law Enf’t Agencies, Guidance for Okla. law enforcement following Dobbs v. Jackson Women’s Health Org, (Aug. 31, 2022) (“Guidance”).
[22] See ibid.
[23]63 Okla. Stat. §§ 1-745.34(A).
[24] 63 Okla. Stat. §§ 1-745.39(A).
[25] See 63 Okla. Stat. §§ 1-745.51-60; 63 Okla. Stat. §§ 1-745.51-52.
[26] Oklahoma S.B. 1555.
[27] 21 Okla. Stat. § 861.
[28] 63 Okla. Stat. § 1-731.4.
[30] See, e.g., 59 Okla. Stat. §§ 509, 509.1 (providing for professional sanctions against physicians).
[31] For clinicians, see e.g., 59 Okla. Stat. §§ 509, 509.1.
[32] 63 Okla. Stat. § 1-731.4; 63 Okla. Stat. §§ 1-745.51-52.
[33] 63 Okla. Stat. § 1-745.31.
[34] 21 Okla. Stat. § 861.
[35] 21 Okla. Stat § 691.
[36] 63 Okla. Stat. § 1-745.52
[37] See Gender Equity Pol. Inst., The State of Reproductive Health in the United States: The End of Roe and the Perilous Road Ahead for Women in the Dobbs Era (Jan. 19, 2023) at 6, https://thegepi.org/wp-content/uploads/2023/01/GEPI-State-Repro-Health-Report.pdf; Donna L. Hoyert, Maternal Mortality Rates in the United States, 2021, CDC (Mar. 2023), https://www.cdc.gov/nchs/data/hestat/maternal-mortality/2021/maternal-mortality-rates-2021.htm.
[38] Katherine Ellison and Nina Martin, “Severe Complications for Women During Childbirth Are Skyrocketing — and Could Often Be Prevented,” ProPublica (Dec. 22, 2017),https://www.propublica.org/article/severe-complications-for-women-during-childbirth-are-skyrocketing-and-could-often-be-prevented.
[39] See, e.g.,Jamila K. Taylor, Structural Racism and Maternal Health Among Black Women,48 J. L., Med. & Ethics 506 (2020), https://doi.org/10.1177/1073110520958875; Saraswathi Vedam et al., The Giving Voice to Mothers Study: Inequity and Mistreatment During Pregnancy and Childbirth in the United States,16 Reprod. Health, 77 (2019), https://doi.org/10.1186/s12978-019-0729-2; Judith A. Lothian, The Continued Mistreatment of Women During Pregnancy and Childbirth, 28 J. Perinatal Educ., 183 (2019), DOI: 10.1891/1058-1243.28.4.183.
[40] See Gender Equity Policy Institute, supra note 37 at 3.
[41] Ibid. at 8-10.
[42] Ibid.
[43] Okla. State Dep’t of Health, Okla. Maternal Mortality Rev. Comm., Oklahoma Maternal Health, Morbidity and Mortality: Annual Report 2021, at 5, 26 (2021),
https://oklahoma.gov/content/dam/ok/en/health/health2/aem-documents/family-health/maternal-and-child-health/maternal-mortality/maternal-morbidity-mortality-annual-report-2021.pdf.
[44] Okla. State Dep’t of Health, Okla. Maternal Mortality Rev. Comm., Maternal Mortality in Oklahoma 2004-2018, at 4 (2020), https://oklahoma.gov/content/dam/ok/en/health/health2/aem-documents/family-health/maternal-and-child-health/maternal-mortality/annual-mmrc-report.pdf.
[45] Ibid.
[46] Notably, the study does not address the larger population of people whose rights to abortion have also been affected by Oklahoma’s legal regime, such as those seeking non-emergency abortions due to other medical conditions or fetal anomalies.
[47] This research methodology is also referred to as a “secret shopper” methodology and has been used as well in multiple consumer and employment studies to document discrimination based on gender, race, and ethnicity (e.g., in examining housing practices based on the race of a prospective renter or buyer).
[48] See, e.g., Pooja A. Lagisetty et al., Access to Primary Care Clinics for Patients With Chronic Pain Receiving Opioids, 2 Jama Network Open (Jul. 3, 2019), doi: 10.1001/jamanetworkopen; Brent R. Asplin et al, Insurance status and access to urgent ambulatory care follow-up appointments, 29 J. of the Am. Med. Ass’n 1248-1254 (Sep. 14, 2005), doi:10.1001/jama.294.10.1248; Karin V. Rhodes & Franklin G. Miller, Simulated patient studies: an ethical analysis, 90 The Milbank Q. 706-724 (Dec. 2012), doi: 10.1111/j.1468-0009.2012.00680.x.
[49] PHR’s Ethics Review Board provided guidance and approved this study based on regulations outlined in Title 45 CFR Part 46, which are used by academic Institutional Review Boards in the United States. All of PHR’s research and investigations involving human subjects are conducted in accordance with the Declaration of Helsinki 2000, a statement of ethical principles for medical research involving human subjects, including research on identifiable human material and data.
[50] See Oklahoma Hospital Directory, Oklahoma Hospital Ass’n, https://www.okoha.com/OHA/Hospital_Directories/OHA/Directory/Hospital_List_Public.aspx?hkey=d87455ef-ec45-49ac-8fd6-fff05ad0116c; Hospitals and Medical Facilities in Oklahoma, OfficialUSA.com https://www.officialusa.com/stateguides/health/hospitals/oklahoma.html.
[51] The Hyde Amendment is a legislative provision, included in Congressional spending bills since 1976, that prohibits federal funds from covering abortion services for people enrolled in Medicaid, Medicare, and CHIP. As a result, Medicaid enrollees are not covered for abortion services in the 34 states (and Washington, D.C.) that do not allocate state funds to extend coverage. Currently, 7.8 million women aged 15-49 with Medicaid coverage lack abortion coverage. Half of those affected are women of color. See The Hyde Amendment: A Discriminatory Ban on Insurance Coverage of Abortion, Guttmacher Inst.(May 2021), https://www.guttmacher.org/fact-sheet/hyde-amendment.
[52] Using the definitions given by the U.S. Census Bureau, hospitals are classified as “heavily urbanized” if the town population exceeds 50,000 people. The “non-urban” category combines the “urban cluster” (2,500 – 50,000 people) and “rural” (less than 2,500 people) definitions to create a large enough sample size. See 2010 Census Urban and Rural Classification and Urban Area Criteria, United States Census Bureau, https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural/2010-urban-rural.html.
[53] Hospitals with fewer than 100 beds in their entire facilities are classified as “small,” those with between 100 and 500 beds are coded as “medium,” and those with more than 500 beds are considered “large.”
[54] Facilities were divided into the following regions, based on their proximity to major urban centers: “Northern” hospitals were those located in the Tulsa metropolitan area; “Central” hospitals were those located in the Oklahoma City metropolitan area; “Eastern” hospitals were those south of Tulsa and east of Oklahoma City; and “Southern” and “Western” hospitals were located south and west, respectively, of the Oklahoma City metropolitan area. All hospital names, locations, and other potentially identifying information have been de-identified in this report.
[55] For the purpose of this study, the team opted to portray the pregnant patients as cisgender women.
[56] Oklahoma Uninsured Fast Facts CY 2021, Oklahoma Health Authority (Nov. 28, 2022), https://oklahoma.gov/content/dam/ok/en/okhca/docs/research/data-and-reports/fast-facts/2023/january/Uninsured%20Fast%20Fact%20CY2021_nov2022.pdf.
[57] Procedures to remove ectopic pregnancies should not be considered “abortions” because the implanted egg is never viable and always poses a life-threatening danger that must be terminated as soon as possible. Failing to make this distinction suggests that ectopic pregnancies fall under the abortion legal framework, which would require doctors to wait until the patient enters a life-threatening state, at which point it could be too late to act. This confusion could be exacerbated by the fact that one of the abortion bans explicitly includes a separate exception for ectopic pregnancies, even though management of an ectopic pregnancy is not medically considered an abortion, while the other bans are silent on cases of ectopic pregnancy. See Tubal Ectopic Pregnancy, ACOG, (Mar. 18, 2018), https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2018/03/tubal-ectopic-pregnancy.
[58] See, e.g., Understanding and Navigating Medical Emergency Exceptions, supra note 10; Abortion Policy: Statement of Policy, ACOG, (May 2022), https://www.acog.org/clinical-information/policy-and-position-statements/statements-of-policy/2022/abortion-policy; Questions to Help Hospital Systems Prepare for the Widespread and Devastating Impacts of a Post-Roe Legal Landscape, ACOG, (Jun. 24, 2022), https://www.acog.org/news/news-articles/2022/06/questions-to-help-hospital-systems-prepare-for-the-widespread-and-devastating-impacts-of-a-post-roe-legal-landscape.
[59] The United States has ratified three core human rights treaties with important protections for reproductive autonomy: the International Covenant on Civil and Political Rights (ICCPR), opened for signature Dec. 19, 1966, 99 U.N.T.S. 171; the Convention Against Torture and Other Cruel, Inhuman, or Degrading Treatment or Punishment (CAT), opened for signature Dec. 10, 1984, 1465 U.N.T.S. 85; and the Convention on the Elimination of All Forms of Racial Discrimination (CERD), opened for signature Dec. 21, 1965, 660 U.N.T.S. 195. The United States has signed but not yet ratified several other human rights treaties that likewise contain critical protections for reproductive autonomy, including the International Covenant on Economic, Social and Cultural Rights (ICESCR), opened for signature Dec. 16, 1966, 993 U.N.T.S. 3; the Convention on the Elimination of All Forms of Discrimination Against Women (CEDAW), opened for signature Dec. 18, 1979, 1249 U.N.T.S. 13; and the Convention on the Rights of Persons with Disabilities (CRPD), adopted on Dec. 13, 2006, 2515 U.N.T.S. 3.
[60] See CRR, Breaking Ground: Treaty Monitoring Bodies on Reproductive Rights 2016, 22 (2016), https://reproductiverights.org/wp-content/uploads/2020/12/GLP_TMB_Booklet_2016_Web.pdf; CRR, Breaking Ground: Treaty Monitoring Bodies on Reproductive Rights 2020, 12 (2019), https://reproductiverights.org/sites/default/files/documents/Breaking-Ground-2020.pdf. See also World Health Organization, Abortion Care Guideline Web Annex A. Key International Human Rights Standards on Abortion (2022), https://apps.who.int/iris/bitstream/handle/10665/349317/9789240039506-eng.pdf.
[61] World Health Organization (WHO), Abortion Care Guideline, 13-14 (2022), https://www.who.int/publications/i/item/9789240039483; CRR, WHO’s New Abortion Guideline: Highlights of Its Law and Policy Recommendations (Mar. 2022), https://reproductiverights.org/wp-content/uploads/2022/03/CRR-Fact-sheet-on-WHO-Guidelines.pdf.
[62] See Comm. on Econ., Soc. and Cultural. Rts., General Comment No. 22: On the right to sexual and reproductive health (Art. 12 of the International Covenant on Economic, Social and Cultural Rights) U.N. Doc. E/C, 12/GC/22 (May 2, 2016) [hereinafter ICESCR, General Comment 22].
[63] ICESCR, General Comment 22 at ¶¶ 12-21.
[64] In the international context, such as in the United Nations, the term “states” refers to national governments (i.e. “state parties”). However, elsewhere in the report, the term “states” is used to refer to the sub-national governments within the United States. See UN Hum. Rts. Comm., General Comment No. 36: On Article 6 of the International Covenant on Civil and Political Rights, on the right to life, U.N. Doc. CCPR/C/GC/36, at ¶ 8 (Sep. 3, 2019), https://www.ohchr.org/sites/default/files/Documents/HRBodies/CCPR/CCPR_C_GC_36.pdf. [hereinafter referred to as HRC, General Comment No. 36]
[65] See generally World Health Organization, Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health (2008), https://apps.who.int/iris/bitstream/handle/10665/43943/9789241563703_eng.pdf;jsessionid=5C0ACAD105BC140CFA4FFFA3CA8F9A31?sequence=1.
[66] Abortion, WHO, (Nov. 15, 2021), https://www.who.int/news-room/fact-sheets/detail/abortion.
[67] See, e.g., HRC, General Comment No. 36; ICESCR General Comment 22; OHCHR, CRC General Comment No. 4: Adolescent health and development, UN Doc. CRC/GC/2003/4 (Jul. 1, 2003); CEDAW, General Recommendation No. 34, on the Rights of rural women, UN Doc. CEDAW/C/GC/34 (2016). See also Special Rapporteur on extrajudicial, summary or arbitrary executions, Report of the Special Rapporteur on extrajudicial, summary or arbitrary executions on a gender-sensitive approach to arbitrary killings, UN Doc. A/HRC/35/23 (2017) (“States should remove undue restrictions on access to safe and legal abortions that may threaten women and girls’ right to life and to health”).
[68] See HRC, General Comment No. 36, at ¶ 8.
[69] See Brief for UN Mandate Holders as Amici Curiae Supporting Respondents, Dobbs v. Jackson Women’s Health Org., No. 19-1392 (U.S. Sep. 20, 2021), at 31-32.
[70] See, e.g., ICESCR, General Comment 22, at ¶ 18; Committee on the Rights of Persons with Disabilities, General Comment No. 3: Women and Girls with disabilities, ¶ 40; Convention on the Elimination of All Forms of Discrimination Against Women (CEDAW), Art. 10, ¶ H; CEDAW Committee, General Recommendation No. 24, ¶ 28. See also ICCPR, art. 19, ¶ 2.
[71] Interim report of the Special Rapporteur on the right of everyone to the highest attainable standard of physical and mental health, UN Doc. A/66/254 (2011), https://undocs.org/en/A/66/254.
[72] ICESCR, General Comment 22, at ¶¶18-21, 40-41, 43-44.
[73] Ibid, at ¶¶ 18-21, 44.
[74] ICESCR General Comment 22, at ¶ 19; HRC, General Comment No. 36, ¶ 8; Committee on the Rights of the Child, Concluding Observations: Slovakia, ¶ 41(e), U.N. Doc. CRC/C/SVK/CO/3-5 (2016).
[75] See ICESCR, General Comment 22, at ¶ 18-21.
[76] See CRR, Breaking Ground: 2020, supra note 60, at 12-15.
[77] Ibid. at 14.
[78] See Hum. Rts. Comm., Siobhán Whelan v Ireland: Views Adopted by the Committee Under Article 5 (4) of the Optional Protocol, Concerning Communication No. 2425/2014, ¶¶ 7.5–7.7, 7.9, 7.11–7.12, U.N. Doc. CCPR/C/119/D/2425/2014 (2017); Hum. Rts. Comm., Amanda Jane Mellet v Ireland: Views Adopted by the Committee under Article 5 (4) of the Optional Protocol, Concerning Communication No. 2324/2013, ¶¶ 7.4–7.6, 7.8, 7.10–7.11, U.N. Doc. CCPR/C/116/D/2324/2013 (2016).
[79] See Hum. Rts. Comm., Mellet v Ireland, Comm. No. 2324/2013, UN Doc. CCPR/C/116/D/2324/2013 (2016). See also CRR, Breaking ground: 2020, at 13, 25. See also Johanna B. Fine et al., The role of international human rights norms in the liberalization of abortion laws globally, Health and Human Rights Journal (2017), www.hhrjournal.org/2017/06/the-role-of-international-human-rights-norms-in-the-liberalization-of-abortion-laws-globally/.
[80] Kamala Chandrakirana, Chair-Rapporteur of the Working Grp. on the Issue of Discrimination against Women in Law and in Practice et al., International Safe Abortion Day – Thursday 28 September 2017, UN Office of the High Comm. For Hum Rts. (Sep. 27, 2017), www.ohchr.org/EN/NewsEvents/Pages/DisplayNews.aspx?NewsID=22167&LangID=E; CRPD and CEDAW, Guaranteeing sexual and reproductive health and rights for all women, in particular women with disabilities (Aug. 29, 2018), https://www.ohchr.org/en/treaty-bodies/crpd/statements-declarations-and-observations; Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, Interim rep. of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, transmitted by Note of the Secretary-General, ¶ 65(h), (i), UN Doc. A/66/254 (2011); CEDAW, Concluding Observations on the combined eighth and ninth periodic reports of Haiti, UN Doc. CEDAW/C/HTI/CO/8-9 (2016); CEDAW, Concluding observations on the combined seventh and eighth periodic reports of Honduras, UN Doc. CEDAW/C/HND/CO/7-8 (2016). See also CRC, Concluding Observations on the combined fourth and fifth periodic reports of Mexico, UN Doc. CRC/C/MEX/CO/4-5 (2015).
[81] Michelle Bachelet, Comment by UN High Commissioner for Human Rights Michelle Bachelet on US Supreme Court Ruling on Dobbs v Jackson Women’s Health Organization (Jun. 24, 2022), https://www.ohchr.org/en/statements/2022/06/bachelet-us-ruling-dobbs-v-jackson-womens-health-organization.
[82] Melissa Upreti et al., Joint Web Statement by UN Human Rights Experts on Supreme Court Decision to Strike Down Roe v. Wade, Working Grp. on Discrimination Against Women and Girls, Special Rapporteur on the Right of Everyone to the Enjoyment of the Highest Attainable Standard of Physical and Mental Health & Special Rapporteur on Violence Against Women, Its Causes and Consequences, (Jun. 24, 2022), https://www.ohchr.org/en/statements/2022/06/joint-web-statement-un-human-rights-experts-supreme-court-decision-strike-down.
[83] CERD., Concluding observations on the combined tenth to twelfth reports of the United States of America, ¶¶ 35-36, CERD/C/USA/CO/10-12 (Aug. 30, 2022).
[84] Questions to Help Hospital Systems, supra note 58.
[85] Ibid.
[86] Understanding and Navigating Medical Emergency Exceptions, supra note 10.
[87] Abortion Policy: Statement of Policy, supra note 58.
[88] Understanding ACOG’s Policy on Abortion, ACOG, (May 23, 2022), https://www.acog.org/news/news-articles/2022/05/understanding-acog-policy-on-abortion.
[89] More Than 75 Health Care Organizations Release Joint Statement in Opposition to Legislative Interference, ACOG, (Jul. 7, 2022), https://www.acog.org/news/news-releases/2022/07/more-than-75-health-care-organizations-release-joint-statement-in-opposition-to-legislative-interference.
[90] In a July 13, 2022 letter to the Senate Judiciary Committee, Ada D. Stewart, Board Chair, American Academy of Family Physicians, expressed concern that, “Cases…. in which patients experience delay or denial as they seek critical and in some cases lifesaving care, will multiply. The result will be worse health outcomes and greater health disparities nationwide.” See Ada D. Stewart, American Academy of Family Physicians, Testimony to the Hearing on Reproductive Care in a Post-Roe America: Barriers, Challenges, and Threats to Women’s Health, S. Comm. on Health Educ. Lab. & Pensions, 117th Cong. 4 (Jul. 13, 2022), https://www.aafp.org/dam/AAFP/documents/advocacy/prevention/women/TS-SenateHELP-PostRoe-071322.pdf.
[91] Statement: ACNM Condemns SCOTUS Decision, Dobbs v. Jackson Women’s Health Organization, Am. Coll. of Nurse-Midwives (Jun. 24, 2022),https://www.midwife.org/statement-acnm-condemns-scotus-decision-dobbs-v.-jackson-women-s-health-organization.
[92] Ibid.
[93] Press Release, AMA announces new adopted policies, supra note 12.
[94] Kevin B. O’Reilly, AMA holds fast to principle: Reproductive care is health care, AMA, (Nov. 16, 2022), https://www.ama-assn.org/delivering-care/public-health/ama-holds-fast-principle-reproductive-care-health-care.
[95] Press Release, AMA announces new adopted policies, supra note 12.
[96] Allen v. Harrison, 374 P.3d 812, ¶ 10 (2016).
[97] Scott v. Bradford, 606 P.2d 554, ¶ 18 (1979) (internal quotation omitted).
[98] 63 Okla. Stat. §§ 1-745.39(A).
[99] Brief for Am. Coll. of Obstetricians and Gynecologists, Am. Med. Ass’n, Okla. State Med. Ass’n, Soc’y for Maternal-Fetal Med. as Amici Curiae Supporting Respondents, Oklahoma Call for Reproductive Justice et al. v. John O’Conner et al., No. PR-120543 (filed Sep. 21, 2022), https://www.ocpathink.org/uploads/assets/pdfs/1053478446-20220921-144041.pdf; Oklahoma Const. art. II, § 2.
[100] Ibid.
[101] Stephen F. Hanlon, Res.Am. Bar Ass’n (Feb. 14, 2005), https://www.americanbar.org/content/dam/aba/directories/policy/midyear-2005/2005_my_104.pdf.
Human Rights Crisis: Abortion in the United States After Dobbs
Following the United States (US) Supreme Court decision in Dobbs v. Jackson Women’s Health Organization in June 2022, people in the US who can become pregnant are facing an unprecedented human rights crisis. In Dobbs, the Supreme Court overturned the constitutionally protected right to access abortion, leaving the question of whether and how to regulate abortion to individual states. Approximately 22 million women and girls of reproductive age in the US now live in states where abortion access is heavily restricted, and often totally inaccessible. This briefing paper details the intensifying human rights emergency caused by the decision, and discusses the ways that Dobbs contravenes the US’ international human rights obligations.
PHR Delegation Brings Evidence and Advocacy to the 52nd Session of the UN Human Rights Council
As we mark World Health Day, PHR continues the fight for health and human rights on the global stage
The United Nations Human Rights Council’s 52nd session in Geneva concluded this week with some meaningful advances for health and human rights. In addition to the adoption of the landmark resolution on the human right to a clean, healthy, and sustainable environment (A/HRC/51/L.7), the Human Rights Council (HRC) also renewed the mandates for several important accountability mechanisms and advanced consensus on some atrocity crimes. Physicians for Human Rights (PHR) was on hand to urge and coordinate action with special mechanisms, diplomats, commissioners of inquiry, and civil society partners.
The delegation, led by PHR’s new Executive Director Saman Zia-Zarifi, with Intern Zena Ahmed and myself, was in Geneva for the fourth week of this session.
With three new major new reports in hand, PHR prioritized the adoption of recommendations related to Syria, Ukraine, Ethiopia, the United States, as well as the global scourge of indiscriminate and misused crowd-control weapons.
Syria
The dire humanitarian and human rights crises in Syria following 12 years of armed conflict was thrown into stark relief this session, as the meeting opened against the devastation of the February 6 earthquake in Syria and Türkiye. PHR’s new report, She Pays the Highest Price: The Toll of Conflict on Sexual and Reproductive Health in Northwest Syria, co-published with the International Rescue Committee (IRC), Syria Relief & Development (SRD) and the Syrian American Medical Society (SAMS), details how ongoing conflict and targeted attacks on hospitals and health care professionals have fueled a crisis in northwest Syria, severely limiting the availability of and access to life-saving sexual and reproductive health services.
The HRC-mandated Independent International Commission of Inquiry on the Syrian Arab Republic released fresh documentation and analysis at this Council session in a new report, exposing “pervasive violations of human rights and humanitarian law across the country.” It also pointed to the pattern of arbitrary arrests, disappearances and deaths in detention across Syria. The HRC signaled its support for such investigative and truth-telling efforts by adopting a resolution to extend the mandate of the Commission of Inquiry on Syria for one more year. PHR and colleagues took the opportunity to offer information to the Commission to advance its important accountability efforts.
PHR also called on States to extend cross-border authorization for unfettered humanitarian access in advance of the July UN Security Council vote on access to the devastated northwest for the almost 5 million people there in need of emergency assistance.
Ukraine
As Russian shelling against Ukrainian civilians and civilian infrastructure continued into its second year, PHR, together with partners, raised the alarm in Geneva about the perpetuation of a pattern of Russian attacks on health in multiple jurisdictions, including in Ukraine. In a new report, released on the one-year mark of the full-scale invasion of Ukraine, PHR, eyeWitness to Atrocities, Insecurity Insight, the Media Initiative for Human Rights, and the Ukrainian Healthcare Center put a spotlight on ten case studies of attacks on hospitals, ambulances and health care professionals in Ukraine, which constitute war crimes and possibly crimes against humanity. Together with colleagues from Insecurity Insight, the Media Initiative for Human Rights and the Ukrainian Healthcare Center, PHR met with diplomats, investigators and humanitarian groups to help translate these independent findings into accountability for perpetrators.
Ethiopia
The Ethiopian authorities have used the Cessation of Hostilities agreement of November 2022 as a pretext to advance a false narrative that violence there has decreased. Through written and oral interventions, PHR and its partners in the embattled region of Tigray put the Council on notice that in fact atrocity crimes persist, with a particularly troubling pattern of targeting adolescent boys for sexual violence. In that connection, PHR particularly welcomed the extension for three years of the mandate of the UN Special Rapporteur on the sale, sexual exploitation and sexual abuse of children at this Council session.
Global Harms of Crowd-Control Weapons
PHR also raised concern about the health harms of crowd-control weapons and their abuse as documented in a new report, Lethal in Disguise 2: How Crowd-Control Weapons Impact Health and Human Rights, co-authored with the International Network of Civil Liberties Organizations (INCLO) and the Omega Research Foundation. In the wake of protests around the world, such as against the murder of George Floyd in the U.S., and drawing on case studies from Australia, Argentina, Colombia, Hong Kong, India, Israel, Kenya, the U.S. and elsewhere, the report concludes that “Law enforcement and security forces have frequently responded to these protests with excessive force and violence that fundamentally undermine the rights to free expression and assembly.”
UN special mechanisms, the World Health Organization, and States involved in developing an international treaty to control the trade in tools of torture used to suppress peaceful protests and abuse detainees are on notice: since 2015 more than 119,000 people worldwide have reported injuries due to chemical irritants like pepper spray and tear gas and at least 14 people have died from the short-range impact of gas canisters. In Geneva, PHR called on them to ban kinetic impact projectiles (KIPs) and other weapons that are inherently indiscriminate or are misused to cause harm.
PHR put all the powers of evidence and persuasion at its disposal at this HRC session to seek remedies for attacks on health care infrastructure and personnel and other issues at the core of its health-based mandate. We’re committed to building on that momentum in the months ahead.
Lethal in Disguise 2
How Crowd-Control Weapons Impact Health and Human Rights
Executive summary
Public protests have surged across the world in recent years, often led by grassroots movements seeking to challenge social and economic injustices, express discontent and demand transformative change from their governments. Economic inequity led to the 2018 “Yellow Vests” protests in France, and echoes of these protests were felt in the 2019 Chile protests, the 2020 Indian farmers’ protests, and those across Colombia in 2021. George Floyd’s 2020 murder by a policeman set off a historic wave of protests across the United States and globally, while similar cases of police brutality were behind the #EndSARS protests in Nigeria.
Protests against authoritarian governments were also seen in places such as Hong Kong in 2019, in Myanmar, Israel and the Occupied Palestinian Territories in 2021, and more recently in Iran, Russia and China in 2022. Recent demonstrations have also played out against the backdrop of the COVID-19 pandemic, in which global protests have occurred in response to perceived government ineptitude or overreach. Whether this pattern of ongoing protests represents a momentary period of turbulence or a new normal is yet to be seen. What is clear is that people-driven protest movements are becoming an increasingly common aspect of the 21st-century geopolitical landscape.
Law enforcement and security forces have frequently responded to these protests with excessive force and violence that fundamentally undermine the rights to free expression and assembly.
Law enforcement and security forces have frequently responded to these protests with excessive force and violence that fundamentally undermine the rights to free expression and assembly. The unnecessary and disproportionate use of force often serves not to disperse crowds and quell dissent but rather leads to acrimony and further escalation of conflict. Such uses of force often involve crowd-control weapons (CCWs), weapons ostensibly designed to inflict sublethal pain on individuals.[1] The rising popularity of CCWs by state actors highlights alarming trends in policing across the world: growing authoritarianism, the militarization of law enforcement, unregulated and precipitous use of weapons against peaceful, unarmed people, politically biased decisions to use force, little transparency around when, how and why CCWs are used and no meaningful accountability. The result is thousands of people worldwide who have been seriously injured or killed by these weapons, and the chilling effect of this violence on millions more.
Rigorous documentation of injuries resulting from the use of CCWs is necessary for understanding their impacts both on health and on assembly, association and free expression rights. In 2016, the International Network of Civil Liberties Organizations (INCLO) and Physicians for Human Rights (PHR) published Lethal in Disguise (LiD1), which was the first report to systematically catalogue the health risks and consequences of CCWs. Our 2016 report leveraged an extensive review of the peer-reviewed medical literature, augmented by reviews of news and human rights organisations’ reports and other data, to elucidate the range and scope of injuries from the use–and misuse–of CCWs.
Since then, the nature, scale, and documentation of protests–and the weapons used–have evolved considerably. There are numerous reports in the media and medical research about thousands of people with severe injuries resulting from CCWs: kinetic impact projectiles (KIPs) have caused permanent blindness, brain damage and internal bleeding; chemical irritants have caused trauma from the canisters, as well as respiratory, skin, and eye injuries from the chemicals; stun grenades have burned people; and acoustic weapons have damaged hearing. Many more injuries likely went unreported.
These accounts and the significant medical and scientific advances that have been published since the initial report’s release demanded that we revisit the findings of LiD1. This updated publication, and the additional resources published on the Lethal in Disguise web platform, aim to advance our understanding of the health impacts of CCWs since the publication of LiD1 and seek to continue to raise awareness about the misuse and abuse of CCWs, the detrimental health effects that these weapons can have, and the impact of their use on the meaningful exercise of assembly, association and free expression rights.
We attempt to answer a number of questions. What has changed in our medical understanding of the consequences of the use and misuse of CCWs globally? What new threats do we recognize these weapons pose not just to health but also to the meaningful exercise of assembly, association and free expression rights? In raising awareness about the misuse of CCWs, we seek to answer these questions and foster a global debate to develop further international standards and guidelines on the deployment of CCWs. Ultimately, our goal is to prevent injury, disability and death by providing information about CCWs and enabling people to exercise assembly, association, and free expression rights safely and freely.
This report examines many categories of CCWs used around the world: including kinetic impact projectiles (KIPs), chemical irritants, water cannons, disorientation devices and acoustic weapons. Because weapons not traditionally considered riot control agents are increasingly being used to police crowds, this report also addresses blunt force weapons (i.e. batons) and new frontiers in CCW technology such as drones, electronic control devices and direct energy weapons. International law concerning the use of force, with specific mention of CCWs, is also discussed.
The title of this update and our prior report is designed to make a fundamental reality clear — CCWs are dangerous and can be lethal. It is time for this to be widely acknowledged. The global use of CCWs by government-controlled security forces on protesters has severe consequences to the physical health of both those targeted and bystanders not targeted, on the mental health of everyone involved, and on the enjoyment and safe exercise of fundamental civil and political rights.
Based on multiple expert interviews, this report also demonstrates that injuries have been repeatedly exacerbated by disproportionate, indiscriminate and excessive use of these weapons. We are not intending to claim that public order and safety are not a legitimate state obligation. Too often, however, the use of force and CCWs are used in violation of local, state and international protocols, resulting in disproportionate and excessive use. Nearly all weapons can and are frequently used as indiscriminate tools of collective punishment against peaceful protesters, bystanders and disruptors alike, regardless of their vulnerabilities, actions or potential for causing harm. Some are inherently unlawful, just because they are indiscriminate.
Police violence is also frequently discriminatory and biased against marginalised groups, including racial, ethnic, political, religious, and other minorities, who too often face disproportionate deployments of force and weapons during protests. While the use of certain CCWs may be warranted in some cases to ensure the safety of the public and law enforcement officials, this study demonstrates that the vast majority of CCWs are not only unnecessary for this purpose, but their use runs directly counter to the objective of “public safety and order”.
Summary of findings
Kinetic impact projectiles[2]
KIPs–commonly referred to as “rubber bullets” or “baton rounds”–are bullet-like missiles used by law enforcement and security forces to deter conduct through the pain of impact. The findings of a systematic review of medical literature indicate that KIPs can cause serious injury, disability, and even death. Our updated research identified 2,190 people with injuries from KIPs reported in medical literature published over the last six years (2016-2021) globally; and at least twelve of the identified people died from their injuries with 945 suffering permanent disabilities. Ocular injuries, including blindness, account for 1,575 of the injuries reported (65% of the total number of injuries).
These data demonstrate that severe injuries are most likely when KIPs are fired at close range, when KIPs contain metallic components or when multi-projectile KIPs are used. Of note, the number of injuries from metal birdshot found in our literature review dwarfs those from other KIPs (82% of all injuries). Additionally, we found that from close range, some types of KIPs have a similar ability to penetrate the skin as conventional live ammunition and can be just as lethal. When launched or fired from afar, these weapons are inaccurate and can strike vulnerable body parts and cause unintended injuries to bystanders, especially when multiple projectiles are scattering from one firearm simultaneously. Our conclusion is that it is doubtful that these weapons can be used in a manner that is both safe and effective in a protest setting.
Key findings on KIPs
- Increase in use and injuries: Since the publication of LiD1, data on the use of KIPs to suppress mass dissent has more clearly illustrated the true health cost of the proliferation of KIPs in law enforcement and security forces worldwide. Focusing on literature published from 2016-2021, 2,190 persons were injured or killed by KIPs, mostly in protest settings, a number greater than LiD1’s total of 1,984 persons reported as injured and killed based on literature published before 2016.
- Multi-projectiles: The finding of widespread injuries from multi-projectile KIPs–where multiple projectiles are fired at once–demonstrates the harmful effects of these inherently indiscriminate weapons. They cannot effectively target a single individual or a single body part, and their use has resulted in serious injuries to targeted individuals (when they impact sensitive body parts) and to bystanders (when the projectiles miss the intended target, instead affecting those not targeted). The results of our analysis suggest that these weapons are more dangerous than single projectiles and leading us to call for a prohibition on their use as a first step in limiting harm from KIPs.
- Metal pellets: The vast majority of reported severe injuries (82%) occurred as a result of metal birdshot, a hunting munition pressed into service in several countries as a KIP. This report illustrates metal pellets’ imprecision, indiscriminate nature, and unmatched capacity to maim.
- “Hybrid” weapons: The development and proliferation of “hybrid” weapons that combine characteristics of KIPs with other CCWs, such as “pepper balls” or stun grenades that disperse rubber balls, are proliferating technologies that must be closely observed and evaluated.
- Canisters misused as KIPs: Tear gas canisters, when fired directly at protesters, can be extraordinarily hazardous. These devices and their resultant injuries are reviewed in the chemical irritants section, but the ad hoc use of other weapons as KIPs must be further examined and regulated.
Chemical irritants
Commonly referred to as “tear gas” and “pepper spray,” chemical irritants include a variety of chemical compounds intended to irritate the senses. The general perception is that these weapons have mostly short-term effects that include irritation of the eyes, dermal pain, respiratory distress, and the psychological effects of disorientation and agitation. A systematic review of medical literature documenting the health effects of chemical irritants identified over 100,000 people who have been injured since 2015. At least fourteen people have died, all of them because of trauma inflicted by the canister.[3] While chemical irritants are often thought of as causing minimal transient harm, our findings also identify longer-term risks, including permanent disability and death from their use and misuse.
Key findings on chemical irritants
- Extensive use, limited evaluation: Tear gas has continued to be used extensively around the world. While chemical irritants continue to be the primary crowd-control agent used by law enforcement and security forces to repress and disperse protests, there is almost no publicly accessible manufacturer or government-sanctioned literature on the composition, health or environmental safety standards on the use of these weapons.
- New ways of deployment: Beyond the use of traditional canisters, sprays, and grenades, the use of chemical irritants diluted in water cannons is a growing problem, with reports of resulting skin irritation and pain. There has also been growing use of other composite weapons, such as pepper balls or water cannons laced with chemical irritants, which complicate the identification of weapons, as well as the treatment of injuries.
- Canisters misused as KIPs: Dense and metallic tear gas canisters can easily cause fatal injuries when fired at the head or torso. All deaths reported in recent medical literature associated with tear gas have occurred due to impacts from military-grade tear gas canisters.
- New hazards recognized as a result of the airborne transmission of viruses, such as COVID-19: The extensive use of chemical irritants during the pandemic has increased the risk of adverse medical effects due to COVID-19’s effects on breathing and the lungs, as well as the risk of infection through induced coughing or sneezing. While there is limited information on the incidence of COVID-19 in the setting of tear gas exposure, this issue continues to be of concern as the pandemic continues, and others will likely follow.
- Psychological impacts: The psychological impacts of the use of CCWs have not been extensively studied nor documented in the medical literature, but cases documented in this review indicate that exposure to chemical irritants may result in significant psychological effects, including potential long-term disability.
Other weapons[4]
Water cannons
Water cannons are inherently indiscriminate, particularly at long distances. They can also make communicating with protesters difficult. Their intimidating size and appearance may cause panic leading to stampedes among protesters. We found that blunt trauma from their force has resulted in blindness, head trauma and fractured bones in a number of people. The use of coloured dyes, chemical irritants, or malodorants in conjunction with a water cannon is a form of collective punishment which underscores the potential for abuse of these weapons.
Disorientation devices
Disorientation devices, also known as “flash-bangs” or stun grenades, create a loud explosion and, in some instances, a bright flash of light. They are made of both metal and plastic parts that may fragment during the explosion and therefore carry risks of blast injuries to targeted individuals and bystanders. Explosions that occur close to people have led to amputation, fractures, burns and death. Additionally, the ability to precisely place these thrown devices is questionable, especially when used in protest settings. There are frequent news reports and anecdotal evidence of injuries and deaths from these weapons, including reports of injuries to military, corrections, and other law enforcement officials while handling these devices.
Acoustic weapons
Acoustic weapons, sometimes called sound cannons or sonic cannons, indiscriminately emit painful, loud sounds that have the potential to cause significant harm to the eardrums and delicate organs of the ears and may cause hearing loss. Eardrum injury and hearing loss have been reported in a handful of lawsuits and other cases; serious questions remain about their safety and efficacy in protest contexts.
Blunt force weapons
Blunt force weapons (i.e. batons) are perhaps the most recognizable police weapon used against protestors. These include many variations of a stick or club, depending on history, culture and context. Batons can be defensive weapons, but in the context of protests, they are frequently used as offensive weapons, sometimes in conjunction with other weapons, to shove, strike, hold or apply pressure on people. Batons, depending on the force and the location of the strike, can cause anything from mere bruising to life-threatening blunt trauma. We highlight cases in Italy, India, Chile and Kenya that illustrate the potential for abuse of batons in protests and demand broad regulation of the use of this type of weapon in protest settings.
New Frontiers[5]
Electronic conduction devices
Electronic conduction devices (ECDs), such as tasers and electric shields, are transitioning from weapons used primarily in arrest or carceral settings to protest contexts. Cardiac arrhythmias, muscle damage and electric burns (both on the skin and internally) may result from electrical conduction, and there may be trauma from the barbs or shields that compounds the danger. ECDs have been identified as contributing factors in over 100 in-custody deaths in the United States as well as thousands of injuries globally. Expanding the use of these weapons to more people poses the risk of far more injuries.
Remotely operated vehicles
Remotely operated vehicles, more commonly known as drones, have seen massive growth in the past decade. Civil liberties experts note that the use of drone technology is the most concerning CCWs development in the past five years. To date, they have been primarily used for surveillance, but they are increasingly being used to carry and fire CCWs. Both of these uses are problematic in terms of injury and the potential to violate fundamental rights.
These weapons may cause additional risk of injury because they can be employed remotely from the actual physical location of law enforcement or security forces, which can limit in-person judgements of how, when, on whom, and how much of a response is appropriate. Mistakes are frequent in military drone strikes, and, by extension, any deployment of drones capable of firing CCWs in protest settings is concerning. To our knowledge, although drones that fire CCWs have only been used by Israeli law enforcement and security forces, a large number of countries have purchased these technologies, leading to concerns about their expanding use.
Access to medical care
The health effects described in this report may be exacerbated by factors that serve to impede access to medical care. These include restricted access to medical transport, forbidding or restricting medical assistance at protests, direct attacks on medical professionals and street medics, and the chilling effect of detaining those injured by CCWs at medical facilities, which leads people not to seek necessary medical attention. These barriers to access to timely medical care have played a significant role in increasing the risk of serious injury, permanent disability, or death from CCWs.
Summary of Recommendations
Since LiD1 was published in 2016, we have seen both improvements and mounting challenges to limiting the dangerous use of CCWs. The initial report was well received and led to numerous national and international discussions around better regulation, resulting in the development of the 2020 United Nations Human Rights Guidance on Less-Lethal Weapons in Law Enforcement (UN Guidance).[6] Protesters are now more aware of potential injuries and have better tools to report on their experiences. At the same time, weapons manufacture and use have proliferated, resulting in more injuries and less accountability for their harm. In many countries, there is still a lack of documentation, reporting and investigation of CCWs injuries. Meaningful accountability for CCWs abuses remains rare.
Protesters are now more aware of potential injuries and have better tools to report on their experiences. At the same time, weapons manufacture and use have proliferated, resulting in more injuries and less accountability for their harm.
In the light of the evidence gathered in this report, INCLO and PHR, with contributions from the Omega Research Foundation, propose several recommendations on all aspects of CCWs use, including: regulating manufacturing and transparency in their design, composition, and testing, to regulating their trade and use; promoting the reporting of all uses of CCWs and seeking accountability for misuse. The purpose of the recommendations, found in detail in Section 4, is to reduce injuries, disabilities and deaths caused by CCWs; to bolster international guidelines for the use of CCWs; to ensure the protection and promotion of assembly, association and free expression rights; to seek accountability in cases of harm; and to develop safe practices for the occasions where these weapons are deployed.
These recommendations are based on two core principles: (1) protecting health and limiting injuries; and (2) ensuring the meaningful exercise of the right of assembly, association and free expression.
Design, development, and procurement
- CCWs and related equipment intended for use in the context of protests must be designed and produced in a way that ensures that they meet legitimate law enforcement objectives and comply with international law and standards. This duty applies to states and their agents as well as to companies that manufacture weapons for law enforcement.
- Information on CCWs, including manufacturer testing data and safety data sheets, must be made publicly accessible.
- International, regional and national controls should be adopted on the trade in CCWs and equipment. These should prohibit the trade in inherently abusive weapons and equipment and control the trade in CCWs that are misused to ensure that they are not used in human rights abuses.
- Testing, evaluation and approval should include a multidisciplinary approach that, in addition to law enforcement and manufacturers, includes policymakers, academics, health professionals and other relevant civil society actors. Testing of CCWs should consider, at the least, legality, level of target accuracy, risk of lethality, risk of serious injury or disability, level of pain inflicted, operational lifespan, reliability (i.e., minimal risk of malfunction) and other relevant factors.
- Selection and procurement of weapons must comply all domestic and international standards, and information about the process and the inventories should be made publicly accessible.
Regulations and training
- States should engage with and support international- and regional-level processes to develop trade controls, including the United Nations (UN) process on controls on the trade in tools of torture.
- Regulations, procedures, and/or protocols on the use of CCWs should be developed for law enforcement based on applicable domestic, regional and international laws. Treaty obligations and international standards should be observed and operationalized in the protocols. These should also reflect the findings from independent testing. Law enforcement should never rely solely on manufacturers’ instructions.
- Law enforcement should be trained in human rights and legal standards as well as human rights-compliant use of CCWs. In addition to teaching the technical aspects of the weapon and its use, training should be contextual, including addressing the specific aspects and challenges of managing protests in compliance with all international, national and local laws.
Use of force
- The use of any kind of force, including CCWs, must always comply with the principles of necessity, proportionality, legality, precaution, non-discrimination, and accountability.
- Appropriate de-escalation techniques should be used to minimise the risk of violence. Law enforcement officials should be aware that even the display of CCWs may escalate tensions during protests. Where force is proportionate and is necessary to achieve a legitimate law enforcement objective, all possible precautionary steps must be taken to avoid, or at least minimise, the risk of injury or death.
- Where a decision to disperse a crowd is taken in conformity with domestic and international law, force should be avoided. Where that is not possible under the circumstances, only the minimum force necessary may be used, with consideration of proportionality, and then only after very clear warnings and opportunities to comply have been made.
Deployment of crowd-control weapons
- This report makes it clear that KIPs can cause serious injuries, permanent disability and even death. Severe injuries are more likely when KIPs are fired at close range. When launched from afar, these weapons are often inaccurate and can strike vulnerable body parts or bystanders. Therefore, the medical evidence in this report underscores that KIPs should never be fired indiscriminately into groups and are, in general, an inappropriate weapon in any protest context.
- Chemical irritants, when deployed using canisters or grenades, are inherently indiscriminate by nature, cause severe pain and injuries and frequently escalate tensions. Therefore, extreme caution must be used before and during deployment, including considerations of the presence of bystanders and the existence of areas of egress and airflow to minimise any risk of overexposure due to serious risk of injury.[7]
- Many CCWs, including water cannons and acoustic weapons, are indiscriminate in nature and must be restricted and, if used at all, used with extreme caution in protest contexts.
- Batons should only be used in exceptional circumstances and only against violent individuals posing significant risks to themselves or others.
- Some weapons have already been determined to cause disproportionate harm to health, undue collective punishment, or both, and must be prohibited. These include any kind of live ammunition; KIPs that fire multiple projectiles at once, also known as “scatter shot” ; any projectiles with metal components or cores, including rubber-coated metal bullets, bean bag rounds and PVC-metal composite material, any projectiles with lead ; and pellet rounds, such as “birdshot”; chemical irritants, including launchers that fire multiple chemical irritant canisters, such as the Venom system, excessively dense or high-grade canisters, canisters with additives or ingredients within them, sprays and grenades that are determined to be toxic or hazardous, have passed their expiration date or are otherwise in disrepair ; dye, chemical irritants or malodorants mixed with or sprayed with water cannons ; disorientation devices, such as stun grenades, explosive grenades or other flash bang weaponry ; direct contact electric shock weapons; some blunt force weapons, such as whips and weighted or spiked batons ; and fully autonomous weapons systems .
- Some weapons are concerning because of the risk of severe injuries or human rights violations. A moratorium on the use of these weapons in protest contexts should be issued until further evidence of their impacts has been collected and the boundaries of their lawful use have been established. These weapons include remotely operated armed drones, the development or use of directed energy weapons, and all other electric shock devices .
- For some weapons, the methods and contexts of use can exacerbate injuries, escalate tensions and compound rights violations. As a result, their methods of use must be restricted and limited. Specifically, firing in enclosed or confined spaces, using excessive quantities, exposing vulnerable individuals, including children, the disabled and older persons, and/or firing weapons directly at individuals or into dense crowds.
Post-deployment procedures and accountability
- Medical care for sick and wounded people must not be restricted or interfered with and identities of those seeking care should not be released to law enforcement .
- Law enforcement officials should record and report any use of CCWs, including specific models of CCWs deployed, the distances from the targeted individuals and/or bystanders and duration of deployment, the number of each type of CCW used, and the specifics of any injuries caused by CCWs. Review of this reporting must confirm that the reporting is accurate, and that the use of CCWs was proportionate, necessary, and lawful .
- There should be a visible identification and a clear chain of command whenever CCWs are used, in order to ensure responsibility and accountability. All decisions taken should be traceable, and those who have taken them must be held accountable .
- All deaths, injuries and suspected misuses of CCWs should be thoroughly investigated by a body independent of the implicated officials, with a view to establishing responsibilities and accountability of the officials involved, including the various levels of the command structure in charge during the incident. Where there is evidence of unlawful conduct, commanders and responsible officers should face administrative disciplinary measures and/or criminal prosecution, as appropriate.
Lethal in Disguise 2: How Crowd-Control Weapons Impact Health and Human Rights is a joint project of the International Network of Civil Liberties Organizations (INCLO) and Physicians for Human Rights (PHR) in collaboration with the Omega Research Foundation (Omega).
ABOUT INCLO
The International Network of Civil Liberties Organizations (INCLO) comprises 15 independent national human rights organizations working to promote fundamental rights and freedoms by supporting and mutually reinforcing the work of member organizations working in their respective countries and collaborating on bilateral and multilateral bases. Each organization is multi-issue, multi-constituency, domestic in focus and independent of government, and advocates on behalf of all people in its country through litigation, legislative campaigning, public education, and grassroots advocacy.
The members of INCLO are Agora International Human Rights Group (Agora) in Russia; the American Civil Liberties Union (ACLU) in the USA; the Association for Civil Rights in Israel (ACRI); the Canadian Civil Liberties Association (CCLA); Centro de Estudios Legales y Sociales (CELS) in Argentina; the Commission for the Disappeared and Victims of Violence (KontraS) in Indonesia; Dejusticia in Colombia; the Egyptian Initiative for Personal Rights (EIPR); the Human Rights Law Centre (HRLC) in Australia; the Human Rights Law Network (HRLN) in India; the Hungarian Civil Liberties Union (HCLU); the Irish Council for Civil Liberties (ICCL); the Kenya Human Rights Commission (KHRC); the Legal Resources Centre (LRC) in South Africa; and Liberty in the United Kingdom.
Police brutality, discrimination, and protest rights are priority areas for INCLO. INCLO members partner to advocate against government and police repression of protests and to promote human rights activism. INCLO also seeks to promote and protect the right to protest by combining technical work–the compilation of standards and analysis–with creating materials intended for a wider audience. Previous reports include: Take Back the Streets: Repression and Criminalization of Protest Around the World (2013); Defending Dissent: Towards State Practices That Protect and Promote the Right to Protest (2018), in partnership with The Global Human Rights Clinic of the University of Chicago Law School; and Protesting During a Pandemic: State Responses During COVID-19 (2021).
The INCLO members that participated in this report are the ACLU, ACRI, Agora, CCLA, CELS, KontraS, Dejusticia, HCLU, HRLC, HRLN, ICCL, KHRC and the LRC. Liberty is not an author or party to the report.
For more information, visit inclo.net.
ABOUT PHR
For nearly 30 years, Physicians for Human Rights (PHR) has used science and medicine to document and call attention to mass atrocities and other severe human rights violations. PHR is a global organization founded on the idea that health professionals, with their specialized skills, ethical duties and credible voices, are uniquely positioned to stop human rights violations.
PHR’s investigations and expertise are used to advocate for the protection of persecuted health workers, prevent torture, document mass atrocities and hold those who violate human rights accountable. In 1999, PHR led the effort to develop the internationally recognized Manual on the Effective Investigation and Documentation of Torture and Other Cruel, Inhuman or Degrading Treatment or Punishment, also known as the Istanbul Protocol, which PHR was instrumental in updating in 2022. PHR has a long history of advocating against weapons that can cause grave injury to civilian populations including organizing against the use of landmines for which PHR shared the Nobel Prize in 1997. As to crowd-control weapons in particular, PHR has assessed the adverse health effects in a number of places, including Bahrain, Egypt, the Occupied Palestinian Territory (OPT), the Republic of Korea (South Korea), Thailand and Türkiye. PHR’s studies have documented severe injuries due to birdshot and rubber bullets in Panama and the OPT, abuse of tear gas posing risks to health in Bahrain, South Korea and Türkiye, as well as beatings using batons and sticks.
Through direct examination of victims, desk research and scientific evaluation of weaponry and its potential adverse consequences (when used both appropriately and inappropriately), PHR has brought relevant information to advocates and policymakers seeking to curtail responses by police and security forces that not only suppress lawful dissent, but also harm human health.
For more information, visit phr.org.
ABOUT OMEGA
Founded in 1990, the Omega Research Foundation (Omega) is a UK-based non-governmental research organisation. Omega investigates and exposes the global manufacture, trade, procurement, and use of a wide range of military, security, and policing weapons, including small arms and light weapons as well as large weapon systems, surveillance technologies, vehicles, and a wide range of law enforcement equipment. Omega works to ensure that human rights and international humanitarian law violations, including torture and other ill-treatment, are not committed or facilitated by people using such equipment and techniques, so that people are free to exercise their full range of human rights without the threat of violence and repression.
Omega’s years of specialist research and investigation have generated an unrivalled source of evidence on equipment used for torture and repression. Using this data, Omega seeks to end the manufacture, trade, and use of inherently abusive weapons, such as batons with metal spikes, which have no lawful use. Omega also strives to strengthen controls on other weapons that are frequently used for repression and human rights violations, including torture and ill-treatment, such as batons, handcuffs, and tear gas. Omega looks to increase transparency and improve controls on the trade of military, security, and policing equipment worldwide.
Omega is working to strengthen use of force standards and their application, support human rights monitors and researchers around the world, force governments to change laws, campaign to control the trade in weapons and equipment, hold corporations and individuals to account, and secure justice for survivors of torture.
For more information, visit omegaresearchfoundation.org.
[1] It is important to note that the violent repression of protesters is not always or solely supported by the use of CCWs. In many countries, including where INCLO member organizations are based (e.g. the United Kingdom), tear gas, water cannons and other CCWs discussed in this report are not used or are banned in the context of peaceful assemblies. However, there are still serious challenges to the full enjoyment of assembly, association and free expression rights.
[2] The health effects of KIPs and chemical irritants are described in detail because there is adequate medical data on associated injuries to conduct a robust analysis. For other weapons, we harness the growing social media landscape and the growth of online news media sources to identify and catalogue injuries reported resulting from weapons.
[3] The deaths reported were primarily in Iraq where military-grade canisters were used.
[4] Although to date there is limited evidence in the medical literature on the safety of water cannons, disorientation devices, acoustic weapons, blunt force weapons (batons) and remotely operated vehicles, case studies involving these weapons demonstrate their capacity for causing significant harm to protesters.
[5] New frontiers in protest contexts include the use of electric weapons (such as tasers) and remotely operated vehicles such as drones.
[6] United Nations Office of the High Commissioner for Human Rights, United Nations Human Rights Guidance on Less-Lethal Weapons in Law Enforcement, 2020 (UN Guidance on LLWs), accessible at: https://www.ohchr.org/Documents/HRBodies/CCPR/LLW_Guidance.pdf.
[7] INCLO member, the ACLU, supports these recommendations and, additionally, calls for a full prohibition of chemical irritants and all indiscriminate CCWs on any mass gathering or assembly. In July 2020, the ACLU submitted a statement to the United Nations Human Rights Council (UNHRC) which among other things stated that: “[p]olice response to protests and other mass assemblies should not involve militarized displays or mass violence by the government, and law enforcement should never deploy indiscriminate weapons, such as tear gas and stun grenades, on any mass gathering or assembly.” Several cities and states in the United States have proposed bills to ban or severely restrict the use of tear gas and/or KIPs in the context of protest. For example, the City of Philadelphia, Pennsylvania, has categorically banned the use of chemical weapons and kinetic energy munitions by the police against any individual engaging in First Amendment activities.