Originally published by Yale Medicine Magazine 2022 Issue 168, “More than skin deep”. Article written by Sumaiya Sayeed.
Of the many reasons to leave one’s home country for a new life elsewhere, war, natural disaster, and violent political or religious persecution are among the worst. For those displaced individuals who have sought a better life in the United States, it can be dispiriting to encounter new barriers: separation from families; crowded detention centers riddled with COVID-19 outbreaks; and seemingly never-ending delays to obtaining legal asylum.
The Yale Center for Asylum Medicine (YCAM), directed by Katherine C. McKenzie, MD, does what it can to alleviate the suffering of asylum-seekers. The faculty members of YCAM use clinical expertise to conduct forensic evaluations, documenting physical and psychological scars people may have acquired before or during their flight to the United States, and write affidavits that outline these findings for use in immigration court. These medical affidavits play a key role in successful legal cases for asylum. In fact, a study showed that asylum-seekers who underwent a medical evaluation were granted asylum at a rate of 89% compared with 37.5% for those who had not.
At YCAM, asylum-seeking individuals are referred to as clients rather than patients, as the clinicians do not provide medical care. These forensic evaluations are performed to produce objective evidence of torture or ill treatment that can be presented in immigration court. In the past year, YCAM has evaluated 17 clients with the help of seven faculty members and 15 students at Yale School of Medicine (YSM) and the School of Nursing.
These medical affidavits play a key role in successful legal cases for asylum. In fact, a study showed that asylum-seekers who underwent a medical evaluation were granted asylum at a rate of 89% compared with 37.5% for those who had not.
Students who assist YCAM faculty members typically review clients’ declaration (in which they describe physical or psychological wounds and their origins) in advance, ask questions during the interview, and photograph or document physical scars. The scars are described, and consistencies with their alleged causes are documented in accordance with the Istanbul Protocol, a set of international guidelines for documenting torture and its consequences adopted by the United Nations in 1999.
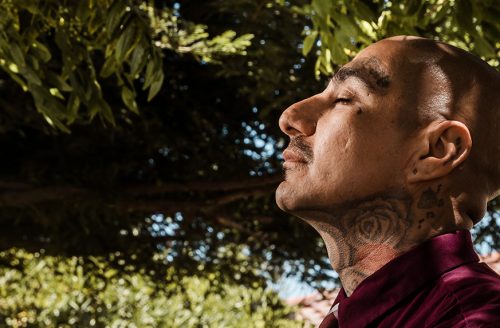
“One client I saw had been tortured with electrocution, leaving them with permanent raised scars on their chest and neck. They shed tears throughout the retelling of their trauma; but after some long pauses and breaks, they persisted, knowing the importance of the medical evaluation in obtaining asylum,” said Rachel Levinson, a medical student at YSM. (Pronouns have been changed to protect the client’s privacy.)
Each client’s story is different, as is every client’s reaction: many show distress or sadness, while others exhibit a flat affect. Often the greatest challenge is anticipating and accommodating the emotional difficulties that a client may experience. “YCAM has taught me the importance of establishing trust with our clients, as it is incredibly triggering to talk about trauma. Learning how to ask the right questions in a trauma-informed way is a skill I am constantly building upon and will continue to sharpen throughout my career,” Levinson said. After the evaluations, the student and faculty member compose a legally valid medical affidavit for the client’s attorney.
“YCAM has taught me the importance of establishing trust with our clients, as it is incredibly triggering to talk about trauma.”
Rachel Levinson, a medical student at YSM
YCAM periodically hosts a training conference for clinicians and students to disseminate information about conducting evaluations of asylum-seekers. In late October 2020, this conference was presented in collaboration with the Society of Refugee Health Care Providers and drew attendees (virtually, due to pandemic restrictions) from across the United States and Canada.
In January 2021, McKenzie and collaborators from other institutions—Hope Ferdowsian, MD, MPH, and Shawn Sidhu, MD—launched the Society of Asylum Medicine (SAM), a broader organization with national scale and scope.
“They had all been doing this advocacy work for asylum-seekers for years, but as they joined forces, they found unmistakable strength and efficiency in working together,” said Niroop Rajashekar, a medical student at YSM. SAM’s main goal is to share resources, educate, and build a community for the professionals and trainees involved in this work. Rajashekar provided essential assistance to group members as they set up the SAM website, key to creating a centralized space in which collaborators in the field can share information and best practices. Beyond being the first organization involved in advocacy work for asylum-seekers to collect training videos, guidelines for medical professionals, and emerging news in one location, SAM has engendered an online community of like-minded individuals comprising medical professionals, mental health care providers, medical students, lawyers, and others.
This year, YCAM collaborated with Physicians for Human Rights (PHR) and the American Civil Liberties Union (ACLU) to research and report on the practice of force-feeding hunger strikers. Together with PHR and ACLU experts, McKenzie and two Yale medical students, Sumaiya Sayeed and John Andrews, detailed the force-feeding taking place in U.S. Immigration and Customs Enforcement (ICE) detention centers. The full report, “Behind Closed Doors: Abuse and Retaliation Against Hunger Strikers in U.S. Immigration Detention,” incorporates information from emails, case records, and interviews pertaining to hunger strikers, many of whom experienced force-feeding and other forms of retaliation while under ICE detention.
“Physicians have the authority to aid asylum-seekers on their legal pathway and a moral obligation to do no harm,” said Andrews. “One of the most startling and disappointing findings of this report was the revelation that some physicians misused their authority to enable force-feeding.” The report calls on medical professionals to advocate for protections for asylum-seekers in detention centers, and to condemn health care workers who may be complicit in involuntary medical procedures and other human rights violations.
The report includes narratives of formerly detained individuals. Their stories, as well as those in the affidavits recorded by YCAM, offer powerful testimony of the ways governments and groups can perpetuate harm against minority populations and individuals.
Creating a space for asylum-seekers to share their stories of persecution relies on the unrelenting passion and clinical skills of YCAM faculty and trainees alike. That YCAM is able to elicit harrowing narratives while providing diligent and objective documentation fulfills its core mission. YCAM continues to expand every year and includes health professionals from the specialties of general internal medicine, gynecology, pediatrics, psychology, and psychiatry. YCAM has adapted both medical and psychological evaluations to safely accommodate clients, faculty, and trainees during the COVID-19 pandemic.