Medical professionals are often on the front lines in conflict situations, providing life-saving health care to civilian communities suffering from violence, abuse, and deprivation. Nowhere has this been truer than in Syria. The targeting of civilians at the hands of the Assad regime and its Russian allies has played a very prominent role in the prosecution of the war, and medical professionals have all too often been violently prevented from carrying out their duties through persecution, arrest, disappearance, torture, and killings.
As first responders, medical personnel also see up close the wounds and evidence of violence and torture that their patients have endured. The government’s persecution of medical professionals is often part of oppressive governments’ intentional strategies of silencing these powerful witnesses.
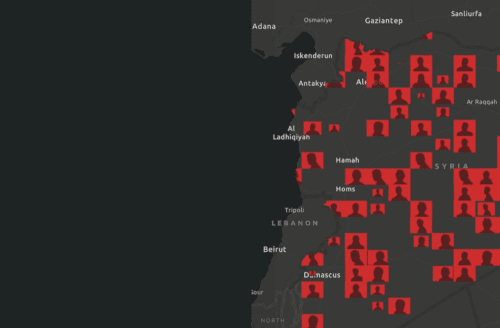
PHR uses open-source data and field sources to document the deaths of medical personnel killed in Syria since March 2011. As of March 2024, thirteen years into the conflict, PHR has assessed that the Syrian government and their Russian allies are responsible for 92 percent of the deaths of medical personnel perpetrated by known actors throughout the conflict. Responsibility for the remaining seven percent lies with non-state armed groups: the self-declared Islamic State (IS), sometimes referred to as ISIS or ISIL, international Forces, and Syrian Democratic Forces. Three events with an unknown perpetrator resulted from attacks launched from areas controlled by both the Syrian government’s forces and the Syrian Democratic Forces. The attacks, which took place on June 12, 2021, targeted al-Shifaa hospital and other civilian targets in Afrin City, Aleppo. The targeting of medical personnel is a violation of international humanitarian law (IHL), and those responsible must be held accountable. When medical workers are killed, the human toll is not just the immediate loss of life, but also the exponential number of people who will suffer or die as a result of not having access to adequate or timely treatment.
-
0
Medical Professionals
At least 949 medical professionals have been killed in Syria from 2011 through March 2024.
-
0%
Personnel Deaths
PHR has assessed that at least 88% of medical personnel killings were committed by Syrian government forces and their Russian allies.
Cumulative Deaths of Medical Personnel
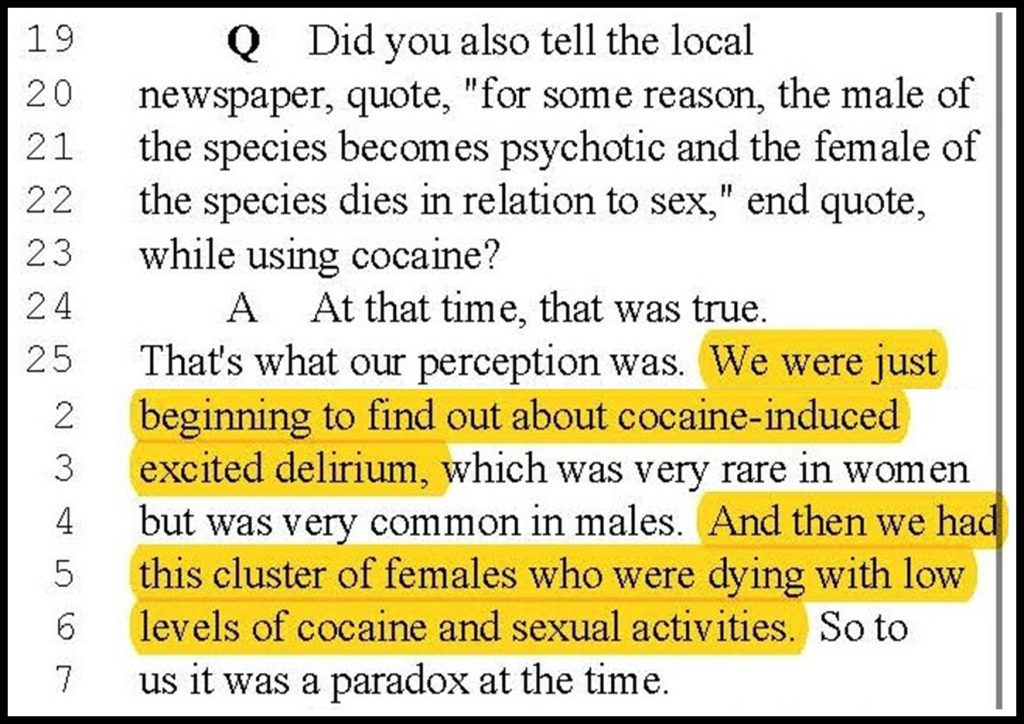
Throughout the conflict in Syria, the Syrian government has systematically targeted medical facilities and personnel, killing doctors, nurses, and others as they care for the sick and injured in hospitals, clinics, and in the field. Health professionals have also been arrested, disappeared, imprisoned, tortured, and executed – often for upholding their professional commitment to treat all patients, regardless of political affiliation. PHR has documented the deaths of 949 medical professionals from the start of the conflict in 2011 through March 2024.
Medical Personnel Deaths Over Time
The beginning of the Syrian conflict was characterized by widespread killings of medical professionals, with 190 killed in 2012 alone. The highest number of killings occurred during the first four years, through shelling, aerial attacks, small arms fire, and the kidnapping and detention of medical workers that often resulted in death through torture or execution. In 2015 in Aleppo, it was reported that over 95 percent of the city’s doctors had fled, been detained, or been killed.
The dip in deaths of medical personnel after 2015 does not necessarily indicate a decrease in the intensity of the conflict, but rather likely reflects a decrease in the total number of medical professionals still in the country.
The targeting of medical personnel is a violation of international humanitarian law (IHL), and those responsible must be held accountable.
PHR recognizes that it cannot know of, let alone corroborate, all attacks on medical personnel. This is illustrated by the Syrian government’s continuous releases of lists of civilians who died in Syrian custody, indicating that there are potentially many more medical professionals who may have died in detention but whose deaths have not yet been made public.
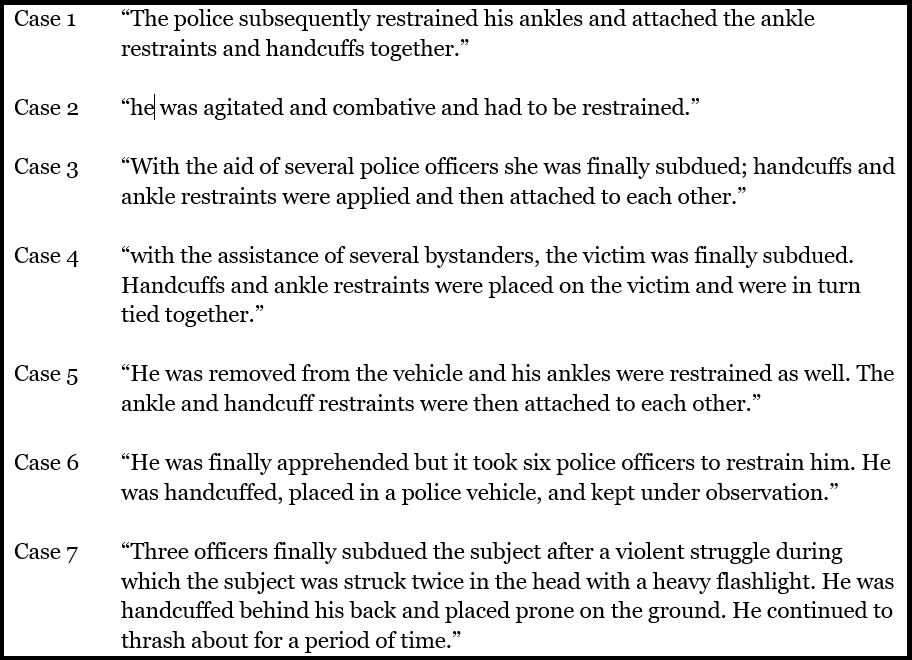
Detention of health care providers has been a deliberate tactic of the Syrian government and part of a broader strategy to weaponize health care as a tool of war. PHR has studied the detention and ill treatment of health care providers in the first two years of the conflict. Our investigations showed that the risk of death in detention centers was higher among those who were detained due to their provision of health care to opposition-affiliated individuals or sympathizers compared to those who were involved in political activities against the government. The data on killed medical personnel shows that 94.3 percent of such deaths were due to detention, kidnapping, torture, and extrajudicial executions perpetrated by the Syrian government from 2011-2015, with a peak in 2012. The strategy then shifted toward targeting health care facilities with shelling and aerial attacks. This resulted in 480 deaths, 81.5 percent of which took place between 2012 and 2016.
Detention of health care providers has been a deliberate tactic of the Syrian government and part of a broader strategy to weaponize health care as a tool of war.
The territorial gains of Syrian government forces since the spring of 2018 have meant a reduction in front lines, and fewer attacks on medical facilities. But even with the changing dynamics of the conflict, medical personnel continue to be targeted for a variety of reasons, including the perception that they are economically advantaged and can be held for ransom. Between 2020 and 2022, 18 medical professionals were assassinated by ISIS and other unknown actors due to the deteriorating security situation, especially in northeast Syria.
Medical Personnel Killed by Governorate
Aleppo, Idlib, and Rif Dimashq represent the governorates with the highest recorded death rates of medical personnel. Spikes in the number of medical personnel killed have tended to coincide with major Syrian government offensives in these governorates.
For example, Aleppo was relentlessly targeted with barrel bombs from 2013 to 2015. In 2016, the Syrian government launched a military campaign to control the city, and by December 22, 2016, it had declared the city “liberated.” During this time, the number of medical personnel killed in Aleppo dropped from a high of 29 in 2016 to five in 2017 and two in 2018 and 2019 combined.
Similarly, in Rif Dimashq, the governorate surrounding Damascus, the Syrian government had been on the offensive since 2013. In April 2018, government forces regained full control over the suburb of eastern Ghouta after a brutal military campaign that killed 20 medical personnel in less than four months. Since then, the number of killed health workers has decreased.
In Idlib, the last rebel enclave in Syria, 85 medical personnel have been killed since 2012. The number increased significantly after 2014, when the Syrian government intensified its military action against various rebel groups who control the majority of Idlib’s countryside. Since the Syrian government and Russia escalated their offensive on the northwest in April 2019, 31 medical personnel have been killed in Idlib, northern Hama, and western Aleppo.
The Numbers Don't Lie
-
0
Of 949 medical personnel killed in the Syrian conflict, at least 280 were physicians
-
0%
Of medical personnel were killed in aerial attacks or shelling
-
0
Medical professionals were either kidnapped or detained, and subsequently killed
-
0%
Of all killings took place between 2012 and 2016
Death of Medical Personnel by Profession
PHR’s definition of “medical personnel” includes doctors, nurses, paramedics, pharmacists, dentists, veterinarians, lab technicians, and health professional students. They must be civilians to be included in the PHR dataset, as medical workers who engage in combat lose their protected status under IHL during such time as they are engaged. As this graph shows, the most affected medical professionals are doctors and nurses, followed closely by paramedics.
PHR chose to include nontraditional medical categories such as veterinarians, dentists, and students because it has received credible reports that these personnel often treat patients due to the lack of licensed physicians and nurses in many localities. The Syrian conflict forced many untrained and under-qualified civilians to step up and take on life-saving roles; according to the recent PHR report, those who volunteered to provide health care among non-physicians were at higher risk of being killed under detention.
The variety of Syrian medical professionals killed across the board points to the systematic destruction of the medical sector and the depletion of medical skills and services throughout the country.
Cause of Death of Medical Personnel
The largest causes of death of medical personnel are aerial bombardment, shelling, and small arms fire. These attacks can be deliberate or indiscriminate, both of which are violations of IHL when directed at medical facilities. As a result of such systematic attacks, many medical professionals died in the line of duty. Many others died after being detained and then tortured and executed.
Due to restrictions in access and limited information, this number is likely to be larger and may continue to increase as families learn that their loved ones died in prisons. In addition, there are many medical professionals who are believed to be alive in detention facilities. These detentions, as well as the concealment of the fate of those who were killed, are gross violations of human rights and humanitarian law.

For Medical Workers in Syria, Impossible Circumstances
For doctors, working in Syria is a triumph of will and determination over impossible conditions. They have been tortured, kidnapped, shot, and shelled. Many have fled while others have stayed behind, placing the lives of their patients ahead of their own. “The obstacles were everywhere,” said Dr. Rami Kalazi, a neurosurgeon who worked in eastern Aleppo city until the summer of 2016. “Massive bombardment everywhere, direct targeting of health facilities, a huge shortage of medical equipment and supplies, especially modern diagnostic devices, a demand for ambulances, a huge lack of medicines, a huge gap in medical experts, very few well-equipped ICUs, few beds in ICUs and wards – besides the enormous number of casualties. Could you imagine the circumstances that physicians in Syria are working under?”

Doctors in the Crosshairs
On March 22, 2011, government forces entered Daraa National Hospital, cleared it of non-essential staff, and positioned snipers on the roof. The snipers remained for two years, firing at the sick and wounded to ensure that only government supporters could enter the hospital. On April 8, a nurse trying to rescue an injured person was shot and killed by government forces in Daraa city. This was just the beginning of the government’s brutal and ongoing campaign of deliberate attacks on medical personnel and facilities as a weapon of war. Read more.

Learning Surgery as the Bombs Fall
In the Syrian government’s relentless assault on health care, nowhere was hit as hard as Aleppo. By the time the city fell to government forces in December 2016, more than two-thirds of the hospitals no longer functioned and roughly 95 percent of doctors had fled, been detained, or killed. Amidst this acute shortage of medical personnel, physicians had to learn to perform new operations on the spot. Dr. K, a dentist who was never trained in maxillofacial surgery, was the only doctor available one day to operate on a patient whose jaw was completely destroyed by a sniper shot. “I had to do deep sutures of the muscle, which was my first time, so I learned by doing that. I closed the patient and hoped that I had done a good job,” he said. Read more.
Timeline

Syrian conflict targets health care
PHR publishes “Syria: Attacks on Doctors, Patients, and Hospitals,” showing that the Syrian government is attacking medical facilities and targeting doctors for treating wounded civilians.

Doctors in the Crosshairs
PHR reports on how the Syrian government is using attacks on medical workers and facilities as a weapon of war. Read more.

Stop Attacks on Doctors in Syria
PHR stages a Die-In near the United Nations in New York to protest attacks on medical care in Syria.

Aleppo Abandoned
PHR’s report reveals that government attacks have devastated health care in Aleppo, where two thirds of hospitals have been put out of service and 95 percent of doctors have fled, been detained, or killed. Read more.

No Peace without Justice in Syria
On the fifth anniversary of the Syria conflict, PHR’s report demands accountability for the Syrian government for war crimes and crimes against humanity. Read more.
Honoring Courageous Syrian Doctors
At our annual gala, PHR honors Dr. Lena and Dr. Nour, Syrian physicians who have risked their lives to provide medical care in Syria and to document human rights abuses. Read more.

Portrait of a Syrian Town Under Siege
PHR’s report show the devastating toll of the Syrian government’s year-long siege of Madaya, which killed at least 86 people by starvation, disease, and traumatic injury, and left just two dentistry students and a veterinarian caring for the town’s 40,000 residents. Read more.

A Deadly Chemical Weapons Attack
CNN’s Christiane Amanpour interviews PHR after our experts identified a probable chemical weapons attack on the town Khan Sheikhoun which killed nearly 100 people, many of them children.

Beyond Imagination: Seven Years of Conflict in Syria
With nearly half a million lives lost and Syria’s health system crippled, PHR renews its call for an end to relentless attacks on civilians and civilian targets. Read more.

“My Only Crime Was That I Was a Doctor”
A major PHR study reveals how health workers have been targeted for detention and torture by Syrian government forces specifically because of their status as care providers.
“Because We Are Doctors”: How Syrian Health Workers Became a Target
Syrian doctor “Youssef” was treating a patient in the hospital when state security forces arrived and arrested him. He is one of dozens of health workers who shared their harrowing stories as part of PHR’s investigations.
Conclusion
After thirteen years of death and destruction, the landscape for human rights, justice, and accountability looks bleak. As of the end of 2023, approximately 15 million people across Syria required health assistance. Many of the health facilities impacted by the conflict remain non-functional. The flight, death, or continued detention of large numbers of health professionals only add to the crippled condition of Syria’s health care system. Furthermore, the devastating earthquake that hit northern Syria last year exacerbated the existing crises endured by Syrians. Addressing the impact of the targeting of health care must begin with justice and accountability for these documented violations of human rights and IHL. Justice must be delivered for medical personnel who were targeted and killed for upholding their civic and moral duty and for those who remain in detention or who have fled Syria and remain too afraid of reprisal to return to their homes and country.
Justice must be delivered for medical personnel who were targeted and killed for upholding their civic and moral duty and for those who remain in detention or who have fled Syria and remain too afraid of reprisal to return to their homes and country.
PHR Methodology for Collection of Data on Attacks on Medical Personnel
PHR utilized open-source data and field sources to document the killing of medical personnel in Syria since March 2011. PHR drew primarily upon the Violations Documentation Center of Syria’s (VDC) English-language website, Syria Network for Human Rights website, media accounts, and social media, corroborating and supplementing this information with data gathered from PHR’s network of physicians in and surrounding Syria. PHR chose to exclude from our data set any documented death identified as a “non-civilian” medical worker, as medical workers engaged in combat lose protected status under IHL.
PHR’s research team collected data from a wide variety of open sources, including United Nations, government, and local and international NGO reports; local, regional, and international news sources; journal articles; Facebook and blog posts; Twitter feeds; and YouTube videos. PHR also conducted interviews and received information and photographs from individuals and organizations involved in providing medical services in Syria and neighboring countries with refugee populations. PHR’s English- and Arabic-speaking analysts reviewed materials in both English and Arabic.
From March 2011 through March 2024, PHR corroborated 604 attacks on at least 400 separate medical facilities and documented the killing of 949 medical personnel. Check out our map of attacks on medical facilities in Syria.
This project is funded in part by ifa (Institut für Auslandsbeziehungen) with resources provided by the German Federal Foreign Office.